|
Fungi are basically simple plants, lacking on chlorophyll
and thriving on other living or dead organisms.
CNS fungus infections have been recognized since the
beginning of this century. Recently they seem to be more frequent as
opportunistic infections in hosts, immunologically compromised.
Immunosuppressive therapy, prolonged use of broad spectrum antibiotics,
drug addictions, diabetes mellitus, renal failure, AIDS and longer
survival of lymphoproliferative malignancies have contributed to the
higher incidence of late. CNS mycoses may also affect the healthy.
Fungi affecting the CNS can be divided into (1) pathogenic
or endemic in healthy host, (histoplasmosis, blastomycosis)
endemic in various part, (2) Opportunistic - in immuno
compromised.
Cryptococus is found in both.
Pathogenesis:
With exception of mucormycosis,
primary site is usually in the lung and rarely in skin. Spread to CNS is
by blood. Rarely there is direct spread from osteomyelitis skull or
vertebrae. Some (aspergillosis) spread directly from nose and para nasal
sinuses.
Pathology:
Manifestations may be due to
(a) Meningitis :
Fungus that primarily causes meningitis is coccidioides immitis,
typically widespread, basal meninges being maximally involved. The basic
lesion is a combination of suppurative and
granulomatous inflammation. This chronic inflammatory response leads to
thickening of meninges, hydrocephalus, arteritis, cranial nerve palsies
and infarction. Other fungi (Blastomyces, histoplasma) may also cause meningitis.
(b) Meningo encephalitis :
Cryptococcus neoformans and the
candida are prone to cause meningoencephalitis. In crypto coccosis, clusters of fungi are spread throughout the
brain, with little or no surrounding inflammatory responses;
predominantly involve basal ganglia and cortical grey matter. The cystic
lesion contains gelatinous poly saccharide which may be detected in CSF
and forms the basis for latex agglutination tests which is 90% sensitive
and highly specific for cryptococcosis.
(c) Abscess/infarction/Hge:
Asperigillus, zygomycetes,
blastomyces, candidiasis cause these lesions as
also nocardia, actinomyces
and coccidioidomycoses. Disseminated
candidiasis produce microabcesses. Vasculitis predispose
to infarction and hge.
Clinical features:
There are no pathognomonic signs and symptoms. In nonendemic areas, history of travel to an endemic
region may give a clue. However specifically affected organs and some
characteristic features help:
(a) Rhino cerebral syndrome presents with orbital pain,
nasal discharge and facial edema. There may be proptosis and visual loss.
Involvement of carotids may cause hemi paresis. Subsequently trigeminal
nerve and adjacent brain may be involved. This is classically found in mucormycosis where blackish necrotic areas are seen
in the palate and nasal turbinates.
(b) Aspergillosis or mucormycosis
may produce sudden onset of deficit due to vasculitis. Rarely there is
SAH due to mycotic aneurismal bleed. Unlike bacterial aneurysms, fungus
affects the larger arteries.
Diagnosis:
Suspicion is the first step.
CSF:
CSF exaination reveals higher
proteins, lower glucose and higher mononuclear leucocytosis.
CSF may be positive for fungi and cultures may be positive, but take a
long time. Candida takes few days, Cryptococci 7 days, while histoplasma and coccidiodes
may take 6 weeks.
Immunological tests:
Latex tests are positive in 90% of crypotococcal
meningitis. In coccidioidomycosis complement
fixating antibody is found in 95%.
|
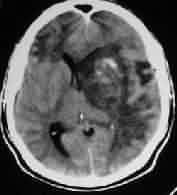
Imaging :
CT & MRI scans show the basal involvement, associated
abscess and areas of infarction and also the status of the ventricles.
|

|

|
|
|
Treatment:
|
Sphenoidal
sinus asperigillosis
|
Intracranial Aspergillosis
|
Intracranial Cladosporiosis
|
(1) Nonspecific measures to lower ICT.
(2) Specific agents commonly used are Amphotericin B, flucytosine and azole derivatives. The duration is
for 4-6 weeks till active systemic or CNS infection has disappeared.
Rifampicin given with amphotericin B potentiates the activity.
(3) Surgical therapy for abscess, hydrocephalus, may be
indicated. Spinal decompression may be required at times.
Intraventricular chemotherapy thro ommaya
reservoir may be tried.
Prognosis:
It depends on the duration and the patient's immunity
status. Without treatment it is a fatal disease.
With Amphotericin B, the mortality has decreased to less
than 50 %
Specific Fungal Infections:
Diffuse:
1. Coccidiodomycosis:
Endemic in south west united states most cases are sub
clinical. Most common in males and agricultural workers. It is primarily
a disease of the healthy and disseminates from a primary pulmonary site
with about 30 - 50% risk of CNS involvement. Focal symptoms are uncommon,
chronic meningitis is common. Bone and joint involvement including
vertebrae occur in about 20%. X-rays reveal radio lucent lesions with
minimal or no new bone formations. Thoracic and lumbar spines are
commonly involved. The disc is relative spared and contiguous ribs may be
involved. Body collapse occur only in late cases, Para spinal masses and
sinus are common.
Amphotericin B in the mainstay. Keto corazole
may help. Overall mortality is about 40% 1 year. Worse in patients with
high intracranial tension. .
2. Cryptococcosis :
It was the commonest CNS fungi, replaced by candidiasis of
late, affects, healthy and immuno compromised.
Primary site is chest. 30 - 50% of disseminated case have CNS
involvement. Meningitis in often the initial presentation. 30% of them
have cranial nerve deficits. Patients are typically afebrile. India Ink
preparation are positive in 60% but the antigen is found in 90% A titre greater than 1:8 is diagnostic. Mortality is
about 30%. Shunting may be indicated in hydrocephalus.
3. Candidiasis :
Candidiasis is rare in healthy. Pulmonary primary is not the
rule. Gastro intestinal urinary or respiratory tract involvement with
subsequent dissemination by blood stream is common. Many enter into the
blood stream via indwelling catheter. Disctitis
following bowel surgery has been reported. CNS involvement is 50% of
disseminated cases and 80% in patients with endocarditis. Meningitis is
common in children, whereas micro or macroabcess
in adults. Serological tests are not reliable. Survival is rare in
patients with abscess formation. Death is usually a result of multiorgan failure.
Focal:
1. Aspergillosis :
Less common and spinal involvement is almost unknown. CNS
involvement is almost unknown. CNS involvement is about 50% of
disseminated cases from primary pulmonary or paranasal sinuses. Clinical
presentation is abscess or mass lesion, meningitis is almost unseen.
Vasculitis leading on to thrombosis and mycotic aneurysms in common
involving proximal larger arteries. CSF findings are nonspecific. Culture
is almost impossible. Few survive with abscess.
2. Mucormycosis :
This fungus is an occasional member of normal nasopharyngeal
flora. It remains nonpathogenic except in patients with diabetic
ketoacidosis in whom rhinocerebral form may
develop. Like aspergillosis there is a strong tendancy
to involve blood vessels. Rhinocerebral mucormycosis begins in the paranasal sinuses, may
extend locally into the orbit with eye pain, facial and periorbital
swelling and ext opthalmoplegia
and proptosis and loss of vision secondary to central artery occlusion.
Vision is usually preserved in most bacterial forms of cavernous sinus
thrombosis. CSF is frequently normal. Death occurs rapidly unlike other
fungal infection.
3. Actinomycosis :
Actinomyces Israeli is responsible. It is
a gram positive, anaerobic intermediate between classical bacteria and
fungi, found in normal oral flora, may become pathogenic in states of
moderate debilitation. The disease has 3 forms, cervicofacial,
pulmonary and abdominal. Pulmonary forms are becoming more common. CNS
involvement occurs in 30-50% as either solitary abscess or purulent
meningitis. Spinal involvement is always secondary to an infection of
contiguous tissue, rarely destroys the discs. Vertebral body destruction
and new bone formation give honey comb appearance. Penicillin for 3 - 4
months is recommended. Prognosis is much better than the true fungi
infection.
4. Nocardia
It is a fungus like (similar to actinomycosis).
gram +ve aerobe. Like
fungi, from a primary pulmonary site dissemination occurs with 50%
involvement of CNS. Single or multiple abscesses which may rupture
causing purulent meningitis. CSF finding are non
specific and culture is difficult. It is penicillin resistant.
Culture is difficult. Gulfomethorazole 4 - 8
m/day for 6 - 12 months is recommended. Mortality is about 80%. Spinal
form is rare.
|