|
Despite the progress in antimicrobial therapy, pyogenic
infections of the CNS remains a serious disease, with significant
mortality and morbidity. The neurosurgeon encounters these infections as
intra-cranial and spinal abscesses and post-traumatic and post-operative
infections. In addition, neurosurgeons are often associated with
management of bacterial meningitis.
1 ) Spontaneous bacterial meningitis:
Almost three-quarters of the spontaneous meningitis are due
to Streptococcus pneumoniae ( pneumococcus ), Haemophilus influenzae (
Haemophilus ) and Nisseria meningococcus infection; certain organisms
tend to predominate with the age of the patient.
|
New born:
|
Childhood:
|
Adult:
|
|
1) Gram negative
bacilli
|
1) Haemophilus
influenzae
|
1) Streptococcus
pneumoniae
|
|
2) Group B
streptococci
|
2) Neisseria
meningitidis
|
2) Neisseria
meningitidis
|
|
3) Listeria
monocytogenes
|
3) Streptococcus
pneumoniae
|
|
Pathogenesis:
Haematogenous spread is the most common,
either venous or arterial. The organisms appear to enter the CSF through
choroid plexus, aggregate in and around cerebral draining veins and
archnoidal villi and cause cerebral phlebitis and arachnoid villous
dysfunction which may lead to increased ICT. Pial cell necrosis, small
vessel arteritis and phlebitis are frequently associated.
Retrograde propagation ( infected thrombi
within emissary veins ) from sinusitis, otitis and mastoiditis and direct
spread from trauma and adjacent infective foci are other modes of
infection.
Clinical features:
The typical symptoms include fever, headache, photophobia,
stiff neck, nausea and vomiting, lethargy or altered mental status.
On examination, in addition to fever, there may be rashes (
meningococcus ).There may be resistance of neck flexion (Kerning's sign )
and passive flexion may cause flexion of hips and knees (Brudzinski's
sign ). Altered sensorium and focal neurological deficit may be noted.
Infants do not usually have neck stiffness.
Examination should also include a search for a primary
focus, such as mastoiditis, sinusitis, otitis and endocarditis.
Diagnosis:
SAH and Neuroleptic malignant syndromes are sometimes
confused with meningitis. Very occasionally a posterior fossa tumor may present
in a similar way. Tuberculous and Viral meningitis may have to be ruled
out only by investigations at times.
Direct examination of the CSF provides the diagnosis.
Decrease in glucose content, elevation of proteins and polymorphonuclear
leukocytosis are the expected findings. A relative increase in
mononuclear leucocytosis or lymphocytes may suggest viral or tuberculous
etiology respectively. Organisms may be detected on a Gram's stain
and grow in culture and their antibiotic sensitivities are essential
for management. AFB staining should be carried out as a routine in these
days of AIDS.
Additional tests such as blood cultures and
counterimmunoelectrophoresis or agglutination tests may help when partial
treatment prevents the growth of bacteria in culture. A lactate content
of more than 3.8 mmol/l in the CSF and C-reactive protein greater than
100 ng/ml will also help in differentiating bacterial from viral
meningitis.
|
A mild diffuse
rise in ICT is common in meningitis and should not prevent a lumbar
puncture. Decrease in the level of consciousness or a focal
neurological deficit suggest presence of increased IC in most. Absence
of papilledema does not exclude a significant increase in ICT.
|

|

|
|
|
|
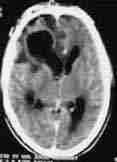
Subdural empyema-rt.frontal&
parafalcine
|
Cerbellar
-epidural abcess
|
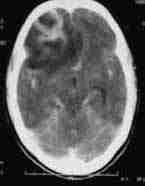
Meningeal
enhancement-CT
|
When suspected, associated intra-cranial abscess or
hydro-cephalus, should be ruled out with CT or MRI scan.
Imaging with CT and MRI is useful in evaluating the leptomeningeal
involvement and complications of meningitis.
Treatment:
Adequate antibiotic therapy, initially empirical, then
according to culture studies is the treatment.
Empirical antibiotic therapy is based on epidemiological
information, age and CSF gram's stain studies and should be started with
broad-spectrum antibiotics. Intrathecal and intraventricular instillation
may be reserved for systemic treatment failure.
Other appropriate supportive management is mandatory. Surgery
may be needed to tide over a crisis, such as hydrocephalus.
Uncomplicated cases require 2 weeks of antibiotics following
a satisfactory response.
Recurrence within a few weeks should prompt a search for a
persistent focus or immune deficiency status. Careful examination for
anomalies such as congenital dermal sinus, enteric cysts,
encephalocele and meningocele is warranted.
2 ) 'Neurosurgical' bacterial meningitis:
Headache, nuchal rigidity and altered sensorium are less
reliable in meningitis in neurosurgical patients. Pre-existing
neurological deficits and effects of surgery may cloud the clinical
picture. They are characterised by different aetiology and require a
different management on occasions.
Post-traumatic:
Streptococcus pneumoniae is more often associated with dural
tears following skull fractures. Penetrating injuries may precipitate
Gram negative bacilli, such as klebsiella, E.coli, Pseudomonas and other
enterobacteriaceae.
Treatment includes surgical repair of the dural tear, in
addition to appropriate antibiotics.
Postoperative:
The incidence of postoperative meningitis varies between
1-15 %. The most common microbes involved were Pseudomonas, Klebsiella,
E.coli and rarely other enterobactericeae.
It is claimed that third generation cephalosporins at the
start of surgery reduce the incidence of post-operative meningitis.
Shunt infections:
The incidence varies in different series with an average of
10%. Staphylococcus epidermidis and aureus (the non pathogenic skin flora
) are often the culprits.
In addition to antibiotic therapy, the shunt may have to be
removed.
Congenital anomalies:
Ruptured meningomyelocoele or a persistent dermal sinus in
the craniospinal axis may be the cause for recurrent meningitis. Unusual
and mixed pathogens should alert the surgeon.
They require appropriate surgery in addition to antibiotics.
3 ) Epidural and subdural empyemas:
These are rare these days.
Epidural empyemas are often
associated with osteomyelitis of the skull. Frontal sinusitis, depressed
fractures and penetrating injuries are the usual causes. Aspiration of
these well localized collections and appropriate antibiotics give good
results. Associated skull osteomyelitis must be eradicated.
Subdural empyemas are an emergency. Paranasal
sinusitis is the common cause. Subdural effusions and hematomas may get
infected and become empyema. Aspiration and appropriate antibiotics is
the treatment. Attention to predisposing factors should follow
immediately.
4 ) Brain abscess:
Incidence is about 8% of the ICSOLs in India and on
the rise in developed countries as well with the advent of AIDS.
Pathogenesis:
Bacteroides and anaerobic streptococci are the most common
causative bacteria.
The majority of them are caused by spread from adjacent
sites. Frontal and ethmoid sinusitis can lead to frontal abscesses,
maxillary sinusitis to temporal lobe abscesses, sphenoid sinusitis to
frontal or temporal abscesses, and mastoiditis to temporal lobe or
cerebellar abscesses. Abscesses from the sinuses are commonly caused by Streptococci.
Those of otic origin is mostly by a combination of aerobes
and anaerobes and is the commonest cause in India.
Trauma, especially with retained foreign
bodies, is also a significant cause. Staphylococcus aureus is
often the causative organism.
Metastatic abscesses from a remote
site are by hematogenous route, the commonest cause in developed
countries. They are often multiple and typically occur at the junction of
the white and gray matter, where the capillary blood flow is the slowest.
They are more commonly seen in the distribution of the middle cerebral
arteries and the parietal lobes, where the regional blood flow is the
highest. The common systemic sites are chronic pulmonary infections, skin
pustules, bacterial endocarditis and osteomyelitis. Those with a right to
left vascular shunt as a result of congenital heart disease or pulmonary
arteriovenous malformations are particularly susceptible. These abscesses
contain a mixed flora.
In about 25 % of patients, the source is unknown.
As the infection reaches the brain, there is immediate
inflammatory response with edema and increased vasculairty;
thrombophlebitis may block venous drainage and edema worsens; small
vessels get thrombosed; areas of necrosis appear; reactions from the surrounding
brain form a capsule and the infection get localized as the capsule gets
thicker.
It is suggested that there is early cerebritis on days 1 to
3, late cerebritis on days 4 to 9, early capsule formation on days 10 to
13, and late capsule formation after day 14.
Meningitis may precede or complicate an abscess. An abscess
may rupture into the ventricles causing ventriculitis which is often
fatal.
Clinical features:
They mimic any other ICSOL with seizures, focal deficits and
features of raised ICT, such as headache, vomiting. There is no specific
feature. Low grade fever may be seen in some, especially in early stages.
Associated causative conditions may suggest an abscess.
Diagnosis:
Suspicion is the first step.
There may be leucocytosis in early stages; ESR is usually
raised; plasma C-reactive protein is elevated.
CT scan reveals a contrast enhancing ring lesion with
non-enhancing hypodense center and surrounding edema. There may be gas
inside the lesion and ventricular and meningeal enhancement.
|
|
|
|
|
|
frontal
abscess-plain CT
|
frontal
abscess-contrast CT
|
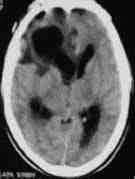
frontal
abscess-ruptured into ventricle-plain CT
|
frontal
abscess-ruptured into ventricle-contrast CT
|
MRI scan delineates the lesion better and also reveals
additional micro-abscesses, if any.
Isotope scan and PET (positron emission tomography ) scan
may be of help to differentiate between an abscess and a tumor with
necrotic
center.
Treatment:
The management is still a controversial topic. Some studies
suggest that with adequate antibiotic therapy, mortality rates (10 to
20%) are similar after aspiration alone, or aspiration followed by
excision, or primary excision.
It is widely presumed that total excision reduces the
recurrence rates and the incidence of seizures, but there is no evidence
to support this .But excision does shorten the hospital stay and the
antibiotic therapy.
Surgical therapy:
Surgery establishes the diagnosis, removes the infected, and
necrotic tissue, provides the material for microbiological studies, and
relieves raised ICT.
The recommended procedures are aspiration, excision and
drainage.
Drainage using a flexible drain is seldom
used nowadays and has been replaced by aspiration and excision
procedures.
Total excision is a must in abscesses containing
foreign material. Excision may be the primary procedure. Some prefer to
aspirate, get the culture studies and excise the lesion after few days of
appropriate antibiotics. Studies suggest that such preoperative
antibiotics are of little benefit. The location and the stage of abscess,
the condition of the patient need to be considered in choosing between
aspiration and excision.
Total excision is not feasible if the capsule is not well
formed or in deep and critical areas without significant morbidity and
also in seriously ill patients. In such cases, stereotactic aspiration
is recommended and it is also useful in multiple abscesses.
Medical therapy:
Blind antibiotic therapy may be of use in ' cerebritis '
stage. There are occasional reports claiming cure with antibiotics alone,
either empirically or after blood and / or CSF studies, especially in
microabscesses. With the advent of stereotactic facilities it is not
recommended even in microabscesses.
Associated antiedema measures and other supportive therapy
are indicated.
Associated predisposing conditions should be eradicated.
Antibiotics should be continued for 6-8 weeks and patient
should be followed up for about 6 months.
5 ) Skull Osteomyelitis:
Most are related to trauma and spread from adjacent sites,
especially the frontal sinusitis. There are occasional case reports of
hematogenous origin.
In acute osteomyelitis, the patient is toxic with tender
swelling over the involved bone called " Pott's puffy tumor "
and likely to involve the CNS.
Chronic ones often present with a lump in the scalp.
Treatment is wide excision of the involved bone until the
normal bone is reached and appropriate antibiotics. Treatment of
associated condition should follow.
6 ) Bacterial infections of the spine:
It is uncommon.
The route of infection is hematogenous from usually the
urinary tract by retrograde venous seeding through Batson's venous
plexus, or direct extension from adjacent sites, or as a result of
penetrating injury. Staphylococcus aureus is the most common organism.
Gram negative organisms and anaerobes have also been implicated.
Iatrogenic causes such as post discectomy (1%), lumbar
punctures are rare. This should be excluded in 'Failed back syndromes'.
It usually affects two adjacent vertebrae and the disc.
Posterior elements are rarely involved. The lumbar and thoracic spines
are more commonly affected.
Acute infections present with fever, backache and tender
spines and the chronic ones with just pain.
Neurological complications, due to epidural extension and
spinal deformity and instability, may occur.
X-rays show disc space narrowing in early stages and
vertebral collapse in late stages with associated deformity.
Isotope and CT scans may pick up early lesions and the skip
lesions. if any.
CT guided aspiration and biopsy for diagnosis and
microbiological studies are widely practiced.
MRI scans reveal the extent of the intra spinal extension.
Treatment is bed rest until pain subsides and antibiotics
are administered for 6 to 8 weeks in uncomplicated cases.
Debridement, decompression and stabilization with bone
grafting is recommended when there is a progressive neurological deficit
and extensive vertebral or intraspinal involvement. Ideally an anterior
or anterolateral approach is employed unless there is posterior
involvement which is rare. Instrumentations are avoided.
|