|
They are also
known as cavernous angioma, cavernous hemangioma and cavernous
malformation. Cavernomas are now more and more frequently
identified in patients with the advent of MRI scanning.
Incidence:
The incidence is about 10% of all cerebrovascular
malformations and about 75% of them are supratentorial and 50% of the
patients harbors multiple lesions.
It has been reported that a sex imbalance exists for extracerebral
cavernomas of the middle fossa, which occur mainly in oriental
female patients. Familial occurrence and multiplicity (10%)
are more frequent in patients of Mexican descent. It has been
recently suggested that the familial form of cavernomas is a
dynamic disease requiring careful monitoring in view of de
novo formation of vascular malformations.
Male patients seem to present with lesions earlier in life
than do female patients . Female patients seem to
be more predisposed to hemorrhage and typically hemorrhage in
the middle decades of life.
Pathology:
These lesions are low flow malformations and consist of
ectatic, largely thrombosed groups of tightly packed, abnormally
thin-walled, small blood vessels that displace normal neurological tissue
in the brain or spinal cord. The vessels are filled with slow-moving or
stagnant blood that is usually clotted or in a state of
decomposition.
There is no definite sex preponderance; however the
incidence of overt hemorrhage is significantly higher in
females. Pregnancy constitutes a well-known risk factor of hemorrhage;
moreover, a major role of endocrine substances in influencing
bleeding and growth of cavernomas has been suggested.
Although cavernous malformations usually do not hemorrhage
as severely as AVMs do, they sometimes leak blood into surrounding neurological
tissues because the walls of the involved blood vessels are extremely
fragile. They are unencapsulated and surrounded by gliotic brain. They
may contain cysts. This non neoplastic lesion may increase in size due to
increase in surrounding gliosis, hemorrhage into cysts or dilated
vascular channels. Calcifications are common.
Like AVMs, cavernous malformations can range in size from a
few fractions of an inch to several inches in diameter, depending on the
number of blood vessels involved. Supratentorial ones are more
frequent.
Some people develop multiple lesions, more so in the
familial variety.
Natural history:
There is no consensus about the natural history as of now.
It has been suggested that some familial, sexual, and racial
factors may play a role in the natural behavior of
cavernomas.
The studies suggest that a subset of lesions
bleeds and bleeds again more frequently and at shorter
intervals than would be expected from the average hemorrhagic
risk; however, the biological profile of these lesions is not
completely defined..
It has been suggested that location may play some
role in the natural behavior of cavernous angiomas. It is not
rare for cavernomas of the third ventricle or in an eloquent
area to demonstrate rapid and extensive growth; hormonal
influence may be the factor or could be related only to the high sensitivity
of these areas even to small bleedings.
The issue of de novo lesion genesis remains
difficult. Some cavernomas probably continue to remain cryptic,
despite the great sensitivity of MR imaging in detecting
these vascular malformations.
The risk of significant bleed is only about 0.2 % per year.
Risk of rebleed is probably similar to that of AVMs.
Clinical features:
Although they are often not as symptomatic as AVMs,
cavernous malformations can cause seizures in some people. In fact seizures are the commonest presenting symptom;
subclinical bleed is the rule. It has been suggested that subclinical
bleeding is the reason for poor seizure
control and that valproic acid may induce bleeding and should be avoided.
Transient neurological deficit is attributed to subclinical
haemorrhages.
In a recent series, the presenting symptoms included overt
hemorrhage in 18%, slowly progressive or transient neurological deficits
in 20.7%, seizures in 46.9%, and headache in 10.3%; 6
patients (4.1%) were asymptomatic.
Investigations:
CT scans may reveal a nonenhancing
hyperdense lesion with no perilesional edema or mass effect, and appears
to fill a void, unless associated with significant haemorrhage.
MRI is more sensitive and specific. A mixed
signal mass because of islands of haematomas of different ages is very
specific. T2 images show a low intensity rim of haemosiderin described as
the ‘target sign’. It has been suggested to be the flow void caused by
tiny draining veins.
|
|

|
|
|
|
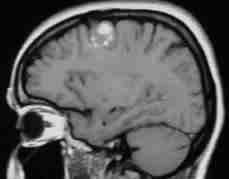
frontal cavernoma-MRI
|
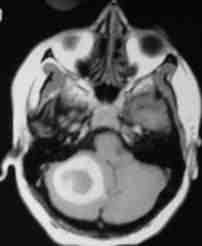
cerebellar
cavernoma
|
hemorrhage due
to cerebellar cavernoma
|
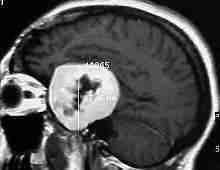
giant
cavernoma
|
GRE images are more sensitive than SE images.
Some MR characteristics of the cavernous angiomas
may help in planning the therapeutic approach; an
increasing hypointense ring around the malformation denotes repeated
microhemorrhages, probably labeling active malformations. Otherwise,
hyperintense lesions on spin-echo MR images denoting subacute
bleeding show a tendency to recurrent hemorrhages.
Angiography may not reveal the lesion
as a rule; however a delayed venous phase may suggest a faint blush in
about 20%.
Management:
|
After AVMs,
cavernous malformations are the type of vascular lesion most likely to
require treatment.
The indications in patients for the surgical treatment
of cavernous angiomas include intractable seizures, progressive
neurological deficits, and previous gross hemorrhage.
Surgical excision of a symptomatic and easily accessible lesion is
advised by most of the surgeons.
There is no consensus on management of incidental,
asymptomatic ones as of now.
|
|

|
|
cav.angioma at surgery
|
|
The choice is between a straight-line approach
through a stereotactic craniotomy or careful microsurgery.
The role of radiosurgery is still being debated. It has been
postulated that the immature endothelium may not be radiosensitive.The
inherent thin-walled structure of the cavernous angioma probably
does not lend itself to the obliterating effects of
radiosurgery on the abnormal vessel of an arteriovenous
malformation.
|