|
Cervical Spondylosis is a non-specific term describing the
morphological manifestations of progressive degeneration of the spine.
SPONDYLO is a Greek word meaning vertebra. Spondylosis
generally mean changes in the vertebral joint characterized by increasing
degeneration of the intervertebral disc with subsequent changes in the
bones and soft tissues.
From the IV to V decade, it is clear that IVD undergoes
progressive desiccation, becomes more compressible and less elastic and
secondary changes ensue. Although the majority of individuals over
40 years of age demonstrate significant radiological evidence, but only a
small percentage develop symptoms. The changes result in neural
compression resulting in radiculopathy or compression of the spinal cord
resulting in myelopathy. Both the neural and spinal cord
compression will result in radiculomyelopathy.
Males predominate for myelopathy. There is no such
proclivity for disc disease.
Etiology and pathophysiology:
The primary event is a progressive decrease in the degree of
hydration resulting in loss of disc height, disc fibrosis and annular
weakening. The extra mobility between adjacent vertebral areas probably
results in osteophyte formation. Though osteophyte formation may be
the body’s attempt to stabilize the joints,
their growth can result in narrowing of the spinal canal and cord
compression.
There are several predisposing factors, which may cause
acceleration of these changes.
(1)
Occupations requiring repetitive motion of the cervical spine.
(2)
Previous injury with fracture or disc prolapse
(3)
Segmentation defects like hemivertebra or fused
vertebrae.
The various factors that play a role in spondylitic
myelopathy are
1) Congenital narrowing of
the cervical spinal canal can be a major cause of myelopathy.
It may be localized or generalized .
Myelopathy is often seen when canal sagittal
diameter is 12 mm or less.
2) Acquired narrowing may be due to
(a) osteophytes
can also cause root sleeve fibrosis due to
irritation.
(b) ossified posterior longitudinal ligament (OPLL)
a well recognized cause in Japan;
may be related to Diffuse Idiopathic Skeletal
Hyperostosis (DISH). Fluorosis may play a part in India;
this heterotopic bone is fragile and the dura may be adherent to this
fragile bone and at risk
during surgery.
(c) Facet joint hypertrophy
may result in foraminal
stenosis and compression of the root and radicular artery
additionally.
(d) hypertrophied ligamentum flavum
may compromise the cord during extension.
3)
Dural adhesions to the posterior longitudinal ligament and the root sleeves
make the cord
more susceptible to injuries.
4)
Vascular compromise by compression of the anterior spinal and radicular
arteries and veins may
be responsible for ischaemia
of the cord and not improve with surgery.
Clinical features:
Neural compression syndromes are
radiculopathy,
myelopathy
or
radiculomyelopathy.
They can be acute,
sub-acute, or chronic and occasionally acute exacerbation of chronic
symptoms can occur.
Radiculopathy refers
to symptoms and signs of nerve root compression such as shooting pain
down the arm, “pins
and needles”
to frank sensory and motor deficits and absence of reflex corresponding
to the nerve root involved. There is
also frequently
referred pain and tenderness along the medial border of the scapula and
in about 60% of patients there
is
occipital headache due to muscle spasm.
The commonest roots
affected are C5 and C6.
Myelopathy has been
classified in various ways and depends on the involvement of the lateral
or medial cord or vascular
involvement. The
signs may be a mixture of upper motor neuron signs in the lower limbs and
lower motor neuron signs in
the
upper limbs and may simulate MND or syringomyelia.
Occasionally the
presentation may be that of Brown-Sequard
syndrome.
Bladder involvement
is unusual.
Combination of
radicular and cord symptoms are found in radiculomyelopathy.
Various autonomic
symptoms can be produced, such as vertigo, flushing, tinnitus and visual
blurring.
These may be mediated by the sympathetic contribution to the sinveretebral nerves from the stellate ganglion.
Vertebro
basilar insufficiency due to spondylitic
compression of the vertebral artery is uncommon, though popularly
diagnosed.
|
Investigations:
The mainstay of imaging is plain X-Rays and MRI.
Plain X-Rays reveal narrowed disc space, and anterior and posterior marginal lipping of
the vertebral bodies. Loss of cervical lordosis is an early
finding. Spinal cord narrowing correlates with myelopathy.
Neurophysiologhical
studies (EMG and nerve conduction studies) can be used when the diagnosis is in doubt. Carpal
tunnel syndrome, thoracic inlet syndrome, amyotrophic lateral sclerosis
may be accurately diagnosed by neurophysiological studies.
MRI is the preferred modality. Apart from clearly
delineating the soft tissue and disc compression it may show signal
intensity changes in the cord itself and helps to assess the degree of
cord damage.
Medical management:
Medical Management mainly targets pain relief. Radiculopathy
improves in majority without the need for surgery. Commonly used
drugs are the NSAIDs and muscle relaxants. The antidepressants may be
useful if functional overlay is marked.
Physiotherapy:
|
|

|

|
|
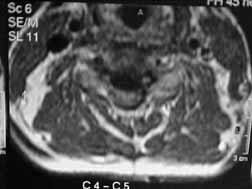
MRI-C-5/C-6
Disc prolapse
|
MRI-Posterior osteo phytes
|
|

|
|
|
MRI-OPLL ( saggital )
|
MRI-OPLL ( Axial )
|
|
Physiotherapy has an
important role adjuvant to medical or surgical treatment. The main
objectives are to decrease the duration of disability, to reduce the use
of drugs and to prevent chronicity and recurrence. Active
modalities such as exercises for the neck, shoulder and the limbs are
preferred.
Passive modalities such as heat, cold, ultrasound, cervical
collar, traction, interferential therapy, etc
should be used only temporarily as an adjunct.
Manipulation should be avoided.
Surgery:
It is indicated when
1.
There is progressive cord dysfunction,
2.
In acute cord compression,
3.
Persistent pain not responding to conservative measures and interfering
with normal life.
Two surgical approaches, anterior and posterior, are
available.
With better imaging and use of surgical microscope, anterior
approach are now used in majority of cases because it is simple and
allows early postoperative mobilization and shorter
hospitalization. In addition, the primary pathology such as disc,
and osteophytes are dealt with directly.
A left sided approach avoids injury to the recurrent laryngeal
nerve injury.
On occasions, such as OPLL it may require drilling of the
vertebral body (corpectomy) for adequate
decompression. Visualization of the posterior longitudinal ligament and a
possible tear, and exploration of the same for extruded disc fragments is
an important step .The presence of such extruded disc fragments may be
suggested by a careful study of the MRI pictures.
When multiple levels (more than two) are involved many
advocate fusion in addition to discectomy. Various techniques are
available.
When root pain is the predominant symptom a fusion to
prevent narrowing of the intervertebral foramen is recommended.
A tricorticate graft obtained from
the posterior iliac crest so that its cancellous part lie against the
subchondral bone above and below the space, while its cortical part forms
the support between the vertebrae (Smith Robinson Technique) is
commonly used.
Attempts to take a graft from the anterior iliac crest may
injure the lateral cutaneous nerve of the thigh.
The drilling the adjacent vertebral surfaces, after removing
the cartilaginous plates, helps in fusion.
The Cloward's technique,
using a bone dowel is also popular.
Simmon's technique
involves making a keystone square in the adjacent vertebral bodies for
the graft.
Bailey and Badgley technique involves making a rectangular trough in the
adjacent bodies for the graft.
Cadaveric bone grafts and methyl methacrylate are used by
some for obvious reasons, but autografts have
been found superior .
Some advocate suturing the prevertebral fascia over the
graft to prevent graft migration.
Some advocate anterior instrumentation in addition to bone
grafting, especially in cases where trauma is a factor. Anterior self locking plate fixation is common. Titanium cage
filled with cancellous bone fixation is specially useful (with or without plates) in
multilevel corpectomy.
|
Post operatively, a hard cervical collar is advised for
six weeks.
Posterior approach may be indicated in canal stenosis,
either congenital or degenerative with hard disc protrusions or
hypertrophy of the ligamentum flavum or multi
segmental OPLL.
C3 to C7 posterior laminectomy is recommended despite the
level of involvement and gives adequate decompression. Additional
foraminotomy (removal of the posterior wall
of the intervertebral foramen) is helpful in myeloradiculopathy.
Occasionally a soft lateral disc protrusion can be removed
through hemi or a partial laminectomy or through an interpedicular
approach.
The complications of an extensive laminectomy are, late
development of spinal deformity and peridural
fibrosis. These can possibly be avoided by expansive laminoplasty. It is performed by completely
incising the laminae on one side and partially on the opposite
side. Elevation with tilting of the lamina upwards on the incised
side allows enlargement of the canal.
Whatever the
surgical approach used, improvement can be expected if symptoms have
been present for less than two years. Results of treatment are also
influenced by the degree of cord compression, changes in signal
intensity of the cord on MRI and number of levels involved.
|
|
|
|
OPLL-Post corpectomy with titanium cage
fixation AP & LAT
|
|
|
|
C-5/C-6 Listhesis
PRE & POST OP
|
|
Radiculopathy improves
dramatically.
In myelopathy, the motor
functions improve faster and better as compared to sensory symptoms.
|