|
Chiari
Malformations:
Hans Chiari first described three
hindbrain disorders associated with hydrocephalus in 1891.
The Type 1 anomaly, which is the mildest,
is characterised by displacement of deformed
cerebellar tonsils more than 5 mm caudally through the foramen magnum.
A number of subgroups have been defined.
In the first group, intrauterine hydrocephalus causes tonsillar
herniation. Patients tend to present in childhood with hydrocephalus and
usually with syringomyelia. A second group
involves those with associated craniocervical
dysgenesis. They usually present later as children or young adults with
occipital headaches especially when straining (cough-laugh headache),
cranial nerve palsies or dissociated sensory abnormalities secondary to syringomyelia. The third group relates to acquired
deformities of the foramen magnum such as basilar invagination. These are
usually adults who develop syringomyelia and
have headaches and cranial neuropathies.
In Type 2, there was in addition, a
displacement of the lower vermis, pons and medulla into the spinal canal
and an elongation of the fourth ventricle from a shallow posterior fossa
through a wide foramen magnum with obstruction to CSF flow at the exits
of the IVth ventricle. Occasionally the IVth ventricle becomes "trapped" or
encysted and will enlarge to appear normal or dilated. Arnold described,
in 1894, a similar malformation of the hindbrain in a case of meningomyelocoele and his pupils Schwalbe and Gredig named the type 2 abnormality of Chiari as the
Arnold Chiari malformation.
Partial or complete agenesis of the
corpus callosum is found in most patients, while falx
hypoplasia, fused enlarged massa intermedia, colpocephaly, abnormal gyral
patterns, and interdigitation of the paramedial gyri across the midline are all associated
features. Infratentorially there is beaking of the tectum, petrous bone scalloping, a low
torcula, and cervicomedullary
kinking. A degree of spinal dysraphism is
usually present with a tethered cord and filum lipoma.
The abnormality is present at birth and
when the meningomyelocele is closed, usually in
the first 24 hours, symptomatic hydrocephalus develops. Signs of brain
stem compression with swallowing difficulties, stridor, apnoeic spells, a weak cry or arm weakness can be
found. If presenting as an adult bilateral limb weakness and wasting
followed by sensory disturbance are most common, with dysphagia and
ataxia being less common.
The type 3 abnormality consisted of
herniation of the cerebellum through a bony defect caused by a cervical
spina bifida. This was really an occipital encephalocoeie,
with the other features of a Chiari II malformation. Patients have severe
neurological defects and a poor prognosis.
Current usage of the "type"
designations also tends to be less rigid; thus, type I cases often show
some downward displacement of the fourth ventricle by magnetic resonance
imaging and on surgical exploration and there is a gradient of
progressively more severe tonsillar ectopia.
It is by no means clear that cerebellar
tonsil displacement is always in the nature of a
"malformation," and numerous instances of cerebellar ectopia following lumbar cerebrospinal fluid shunting
are now documented.
With magnetic resonance imaging, more
recent reports have shown that tonsillar descent is quite common in
children who have undergone lumbar cerebrospinal fluid shunting; syringomyelic cavities may also develop in this
situation.
Pathophysiology:
The various theories which try to
explain the embryogenesis of the Chiari malformation. either
base it on mechanical factors or on a primary dygenesis
of the brainstem. The association of syringomyelia
as seen in 88 per cent of patients of Chiari Type II at autopsy and 75
per cent of Type I Chiari malformation, points towards a common etiology.
The hydrocephalic theory initially
proposed by Chiari in 1896, and resurrected, in 1959, by Gardner
envisaged that the raised pressure due to hydrocephalus pushes the
cerebellum through the foramen magnum. However, a Chiari malformation
without hydrocephalus, or a meningomyelocoele are pointers against this hypothesis.
Penfield and Coburn, and later
Lichtenstein, believed that tethering of the spinal cord by a
myelomeningocele pulled the brain stem and tonsils through the foramen
magnum with axial growth.
A variant of this concept was proposed
by Roth, who envisioned that the myelomeningocele prevents normal
downward migration of the neuraxis, resulting
in an upward push of the cervical-medullary junction with resulting
kinking of the brain stem and "overflow" of the cerebellar
tonsils through the foramen magnum. The experimental work of Goldstein
and Kepes puts such theories in doubt.
Patten’s overgrowth theory postulated
that owing to various noxious stimuli, there was an overgrowth of
developing tissue which leads to an extrusion of the cranial contents
through the foramen magnum. However, the cerebellum of the Chiari
malformation is hypoplastic, not hyperplastic.
Peach postulated that the malformation
occurred as a result of a failure of the pontine flexure to develop. The
medulla gets kinked in the process, with herniation of the hindbrain and
the cerebellum into the cervical canal. The lower pons and upper medulla
are thin and elongated, the lower medulla is thickened and the cerebellum
is hypoplastic. The cervical roots run in an
upward direction. The normal direction of the roots is established only
in the mid-thoracic level. There may be hypoplasia of the falx and tentorium. The foramen magnum may be
deformed and the cervical canal widened. There may be abnormalities of
the septum pellucidum, widening of the massa intermedia, cysts of the third ventricle, beaking of the tectum, forking of the aqueduct, microgyria and upward herniation of the cerebellum.
Padget’s 'Neuroschistic' hypothesis suggests that the
malformation begins as a premature junction of damaged bilateral cerebellar
primordia to form a dysplastic vermis in an already microcephalic
posterior fossa. This is the result of abnormal neural clefts
(neuroschisis) splitting open the primitive
neural tube. These clefts are relatively large and located anywhere
along the spinal axis, but are often caudal and lead to severe types of
spina bifida, as in the Arnold-Chiari malformation (Chiari's type-2). On
this basis, smaller clefts in older embryos with less scarring and less
posterior fossa microcephaly may give rise to the Chiari type-1 entity.
Modern theories suggest that maldevelopment of the para-axial mesoderm of the
fourth occipital sclerotome produces subnormal posterior fossa volume,
while there is no reduction in infratentorial
brain volume, precipitating hindbrain herniation through the foramen
magnum.
Although no gene or gene combination has
been correlated with CMI, familial clustering and an association with
genetic syndromes such as achondroplasia, hypophosphatemic
rickets, Albright's hereditary osteodystrophy, and William's syndrome
provide evidence for a genetic contribution to some cases.
Clinical Picture:
Type I Chiari malformation: In children,
the most common presenting symptom is headache, with or without posterior
cervical pain, Pain may manifest as persistent crying or irritability and
sometimes with hyperextension of the neck or opisthotonos.
In adults and older children, typically
the symptoms are related to syringomyelia with
a suspended and dissociated sensory impairment, with mainly pain and
temperature sense being affected. Pain is the single most common
presenting complaint
Other symptoms have been correlated
with the site of compression. Cerebellar compression may cause ataxia and
nystagmus; brain stem compression may produce pain, dysphagia and facial
numbness. Spinal cord compression, often caused by a syrinx, may cause
pain, weakness and/or sensory changes.
Lower cranial nerve dysfunction is
present in approximately 20% of patients and can manifest as sleep apnea,
dysarthria, hoarseness, recurrent aspiration, and tongue atrophy.
Type II is primarily seen in children
and is almost always associated with a meningomyelocoele
and in 90 per cent of cases with hydrocephalus as well. Chiari II
malformation is the leading cause of death in patients with a myelomeningocoele. Brainstem involvement with
compromise of lower cranial nerves, manifests as respiratory stridor,
sometimes progressing to periods of apnoea and
occasionally death. After infancy the main complaints are related to gait
and limb incoordination spastic quadriparesis
with the involvement of the pyramidal tracts.
Imaging:
Bony abnormalities of the skull and
spine are common even in Chiari Type I-malformation. As many as
two-thirds of patients show an abnormality in the form of larger basal
angles, short clivus, and a reduced posterior
fossa size, supporting the view that tonsillar herniation in these
patients is as a result of occipital dysplasia. Thin cut CT scan with
two-dimensional reconstructions aids in the identification of bony
abnormalities at the cranio-cervical junction.
|
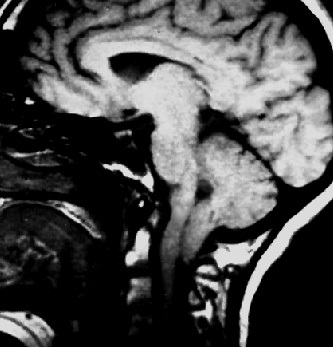
MR is the imaging modality of
choice for diagnosis as well as in the follow up of these patients.
Most clinicians will give a diagnosis of CMI if the cerebellar tonsils
descend 5 mm below the foramen magnum and demonstrate a peg-like
morphology, rather than the normal rounded shape. Using MRI data from
221 patients without hindbrain pathology, Mikulis
and colleagues proposed criteria defining tonsillar ectopia.
During the first decade of life, ectopia
would be present in cases of herniation greater than 6 mm below the
foramen magnum. Role of dynamic MRI is being evaluated. During the
second and third decades, herniation of greater than 5 mm would
constitute ectopia. Although herniation of
greater than 5 mm generally is associated with symptoms, patients who
have as much as 12 mm of tonsillar herniation may be
asymptomatic.
In patients with Chiari type 1
an acquired Chiari caused by a mass lesion or hydrocephalus must be ruled
out. Screening of entire spinal cord to assess for the presence of a
syrinx, scoliosis, or other less common abnormality such as a tethered
cord is mandatory.
|
|
|
|
Chiari type
1-MRI
|
|
The main features of Chiari II are
caudal displacement of the pons, medulla, and fourth ventricle, often with
elongation and kinking. The cerebellar vermis herniates into the cervical
spinal canal through an enlarged foramen magnum, with low-lying tento-rium cerebelli. Cerebellar heterotopias are
also common. Supratentorial anomalies include collicular fusion, which gives the radiological
impression of tectal plate beaking,
and an enlarged massa intermedia. Partial or
total agenesis of the corpus callosum is seen in 33% of cases. Skull
deformities include luckenschadel, scalloping
of the petrous pyramids, clival shortening, and
the previously mentioned enlargement of the foramen magnum.
Other findings are Hydrocephalus(80%)
will develop in more than 80% of infants, syringohydromyelia(48%to
88%) and sccoliosis ( 50% to 90%).
Treatment:
Type 1: With advent of MRI there is
increasing number of asymptomatic patients. The radiological criteria for
the extent of tonsillar herniation are not absolute and should be considered
within the clinicopathological context.
There is a lack of standard treatment
regimens and outcome measures, in the literature. The goal is to restore
normal physiologic CSF flow at the cranio-cervical
junction. Posterior fossa decompression accomplishes this and eliminates
the cranial-spinal CSF pressure differential that likely contributes to
syrinx formation.
Dural opening and intradural
maneuvers, such as amputation of cerebellar tonsils, plugging of the obex, duraplasty, and stent
placement, remain subjects of significant debate. Anderson and
colleagues showed improved nerve conduction through the brain stem occurs
after the bony decompression rather than the dural
opening. There is evidence that the pediatric population responds well to
simple bony decompression without dural opening.
Complications are significantly more frequent in the groups who underwent
dural opening
Patients with mainly pain and minimal
neurological deficit will improve by about 70%. Despite good initial
results, some patients likely will present with recurrent symptoms.
Presence of syringohydromyelia does not appear
to predict the outcome. The only variable predictive of a positive
clinical outcome was age at diagnosis younger than 8 years.
Type 2: Early myelomeningocele repair is
the first operative intervention for almost all infants, and most of them develop fresh symptoms secondary to the
Chiari malformation following surgical repair, In the majority, the
treatment would be quite simple and a ventriculoperitoneal
shunt to take care of the hydrocephalus and brainstem compression. A posterior
decompression is rarely required and when it is required to be performed,
mortality figures approach 40 per cent in the best of hands. During
posterior decompression a cervical laminectomy without removal of the
occipital bone is adequate as the foramen magnum is capacious. Surgery
appears to arrest the neurological deterioration, and generally, the
adults do better.
Syringomyelia(Syrinx):
Syringomyelia is defined as a
cystic cavity in the spinal cord. The term syringomyelia
is generally used in the medical literature today for all cysts of the
spinal cord, with the exception of most cysts associated with
intramedullary tumors whose xanthochromic,
proteinaceous fluid can be regarded as a product of the tumors. Simon
introduced the term ‘hydromyelia’ to describe
distended central canal lined by ependyma,
containing CSF. Syringobulbia represents an
upward extension of the cystic cavity into the brain stem.
Pathophysiology:
Among many etiologies including trauma
and tumors, the most common cause of syringohydromyelia
is Chiari malformations. Chiari believed that fluid was present in the
cord because of persistence of an embryological state: embryological hydromyelia associated with hydrocephalus. Other
earlier theories suggested that the syrinx formation and extension
depend upon open communication between the ventricular system and the
syrinx through the obex.
On reviewing the earlier theories,
Oldfield et al proposed that the impacted cerebellar tonsils act as a
piston, compressing the cervical spinal cord and cranial aspect of the
syrinx with each cardiac cycle.
Dynamic MRI findings demonstrating
pathological obstruction of caudal CSF flow at the cranio-cervical
junction during cardiac systole support this theory. However, an isolated
thoracic syrinx.
and the observation
that syringohydromyelia occurs more commonly
with moderate degrees of tonsillar herniation as opposed to mild or
severe herniation do not support this theory.
Post traumatic syrinx is the commonest
in primary spinal forms. Subarachnoid space compression due to tumor, and subarachnoid space compression or scarring in
relation to spondylitic disease are other
possible causes for a primary spinal syringomyelia.
In has been suggested that tissue
necrosis and hematomyelia occurring after a
cord injury are the precursors of an intramedullary cyst, which
presumably develops as the blood elements are resorbed.
The appearance of post-traumatic spinal
cord cavitation after very minor spinal trauma raises questions about
this theory, or at least its general applicability. It is likely that
subarachnoid scarring develops after trauma and impede rapid pressure
equilibration within the subarachnoid space proximal and distal to the
scar (spinal-spinal pressure dissociation).
Clinical features:
Children with Chiari malformation more
are likely to present with motor or sensory changes or scoliosis.
Adolescents more often present with motor and sensory disturbances,
while younger patients commonly present with scoliosis.
|
Symptomatology in syringmyelia, unassociated with Chiari
malformations depends on the site and etiology. Early in the course of
the disease there is a wide range of fluctuating symptoms and signs,
which often lead to a mistaken diagnosis. Pain in the neck or back,
scoliosis or torticollis may be an early feature. Approximately 80 per
cent of patients complain of stiffness of the lower limbs and weakness
of either the upper or the lower limbs. Intrinsic wasting of the
concerned muscles, dissociated sensory loss, spastic weakness of the
muscles may be other neurological findings. Extension into brainstem
may cause unilateral or bilateral lower cranial nerve palsies, nystagmus,
and wasting of the tongue.
Imaging:
MRI is the choice of imaging, and
delineates associated Chiari malformations, and other associated C-V
junction anomalies.
Contrast myelography
helps when MRI is contraindicated and also in post
traumatic syrinx. Flow of contrast medium under fluoroscopy, may
demonstrate a focal area of subarachnoid scarring, which has direct
implications for the treatment of post traumatic syringomyelia.
Dynamic MR imaging permits a
study of cerebrospinal fluid flow patterns. It is becoming more
important in distinguishing hydrodynamically
active syrinx cavities from cavities with little pulsatile flow, which
may also be expected to show less benefit from surgical therapy.
|
|

|
|
Holocord
syrinx-MRI(T2)
|
|
Treatment:
Treatment of asymptomatic syrinx is
debatable, although majority of pediatric surgeons prefer surgery.
Posterior fossa decompression, corrects
the pathologic CSF flow dynamics associated with Chiari malformation,
leading to syrinx collapse in many cases.
Younger patients do well. The role of
syrinx diversion is controversial, in syrinx associated with Chiari malformations,
and it frequently is used to treat refractory syringomyelia.
In primary spinal forms, historically,
aspiration, drainage, myelotomy, and a variety of devices and tubes, as
well as different extraspinal drainage sites
have been used for diversion of fluid from a syringeal
cavity. Shunting the fluid from the syringeal
cavity to subarchnoid space has been practiced
for many years.
Presence of extensive
subarachnoid space scarring warranted techniques of shunting from
the cyst into the peritoneal or pleural cavities were introduced.
In the presence of injured cord, it is
difficult to evaluate these patients pre or post operatively. Reports
suggest drainage of the syrinx
helps.
Syringomyelia associated with
tumors, obviously, requires tumor excision.
Syringomyelia with archnoiditis do not do well.
|