|
Surgery
for epilepsy is not new. In the mid-seventies, epilepsy surgery took a
dramatic downward trend world over with the introduction of newer
antiepileptic medications. With the advances in neuroimaging and digital
video techniques and data storage, worldwide interest in epilepsy surgery
has increased of late. Today, epilepsy surgery is more effective and
conveys a better seizure control rate. It has become safer and less
invasive, with lower morbidity and mortality rates. Out of 50 million
people with epilepsy globally, one million people with medically
refractory epilepsies, of which nearly one half are potential surgical
candidates in India. This chapter summarizes the current presurgical
evaluation and surgical strategies.
Presurgical
evaluation:
Surgery
is considered when adequate medical treatment in a patient with epilepsy
has failed to give satisfactory control of the attacks, which interfere
significantly with the patient’s ability to lead a normal or near normal
life.
|
The main aim of surgery is to reduce the seizure
frequency rather than “cure” the epilepsy while minimizing the risk of
neurological deficits. Cooperation of the patient and his/ her
relatives is imperative to achieve this goal. Contraindications to
epilepsy surgery include presence of a psychiatric disorder and
progressive neurodegenerative disorder.
The presurgical evaluation should be able to
provide details on the patient’s current neuropsycholgical status,
determining the exact location of seizure activity and evaluating the
surrounding areas of the brain to determine what kinds of problems the
patient might experience after surgery.
The
goal of the presurgical evaluation is to determine if the patient has a
single epileptogenic focus that is not in eloquent cortex, and can
therefore be resected without causing an unacceptable neurological
deficit. The presurgical evaluation for epilepsy (Table 1) has changed
substantially in the past few decades, most notably since the advent of
long term video EEG monitoring and advanced neuroimaging techniques.
|
|
(Table 1) Presurgical evaluation
|
|
Components
|
|
Non invasive
assessment
Clinical
assessment
Brain
imaging
Neurophysiology
Neuropsychology
Invasive
assessment
Carotid
amobarbital test
Intracranial
electrodes
|
|
Clinical
assessment:
The
importance of a good clinical assessment cannot be overemphasized. All
components of seizure signs and symptoms (seizure semiology) should be
evaluated in the assessment. The ictal history will point towards the
origin and spread of seizure activity within the brain whereas the interictal
component of history will indicate the pathology. Seizures and epilepsies
naturally fall into 2 major groups, based on the site of seizure onset in
the brain, either (1) focal (partial, localization-related) or (2)
generalized.
The
signs and symptoms of simple or complex partial seizures arising within
the temporal and frontal lobe easily point to the site of origin.
Seizures arising in primary sensory or motor areas, in other
supplementary areas and in the occipital lobe have a fairly typical
presentation. Some patients may develop transient neurological deficit
following a seizure known as Todd’s paresis.
The
typical candidates for surgery are patients with intractable epilepsy due
to unilateral hemispheric cerebral pathology. Bilateral pathology or
deficits predicts poor seizure-free outcome. The outcome in patients with
an extratemporal seizure focus after resection has been worse than in
those with a temporal focus,probably due to the more diffuse nature of
such lesions.
Brain
imaging:
Routine
skull films are of little value. It may reveal tram track calcification
as seen in tuberous sclerosis. Magnetic resonance imaging (MRI) is the
imaging of choice in epilepsy patients and has replaced routine
computerized tomography (CT) because of superior imaging. CT scanning
demonstrates intraparenchymal calcium and acute bleeding which help in
distinguishing certain types of tumors or CNS syndromes, such as tuberous
sclerosis. An epilepsy syndrome diagnosis combines the seizure type with
its associated MRI, physical examination, genetic and other
features.
Every
presurgical evaluation should include a complete study with special
thin-cut coronal magnified views perpendicular to the axis of the
temporal horn. MRI scanning lessens the need for invasive neurophysiological
recording. Mesial temporal sclerosis varies in its severity and
laterality and the ability to demonstrate this lesion will vary according
to the MRI technique available.
Various
MRI sequences including volumetric analysis and fluid-attenuated
inversion recovery (FLAIR) sequences are now available especially to
study the temporal lobes in suspected cases of mesial temporal lobe
epilepsy and demonstrate subtle changes. Cortical neuronal migration
disorder can exist in diverse forms, some of which are amenable to focal
resective surgery and others which are not. MRI can also
show when pathology is more widespread or multiple or when there may be
dual pathology. MR spectroscopy may be used as an adjunctive to the other
data.
If
neuro-imaging demonstrates a well-characterized lesion (i.e. unilateral
hippocampal atrophy, cavernous angioma, focal cortical dysplasia, etc.)
supporting the clinical features of the seizures, surgery may be
reasonable without the general requirement for ictal EEG data or further
imaging.
Functional
Brain Imaging:
Positron emission tomography (PET) measures
regional cerebral metabolism and blood flow. Fluorodeoxyglucose (FDG) is
most commonly used metabolic substrate for PET scan. Ictal PET is not
practical due to the extemely short half life of the radiotracers used.
In temporal lobe epilepsy (TLE), in the interictal state, there may be an
area of hypometabolism on the same side as the epileptic focus. PET is
more useful for lateralizing than localizing the epileptic focus. Patients
with bilateral hypometabolism on FDG-PET have a worse outcome from
temporal lobe surgery than those with unilateral hypometabolism.
Single-photon
emission tomography (SPECT) demonstrates regional cerebral blood flow,
which is linked to cerebral metabolism and can therefore be used to
identify the epileptic focus. Hexamethylene propylene amine
(HMPAO), used for SPECT studies, is stable for several hours, allowing
delayed imaging. It is useful to identify the offending epileptiform
focus in patients with multiple pathologies for example tuberous
sclerosis. SPECT studies are obtained by injecting the radiotracer during
(ictal) or soon after (postictal) the seizure activity. Co-registration
of SPECT on MRI is being used in some centers. SPECT is less reliable
than interictal PET for identifying dysfunctional cortex with
hypometabolism.
Functional MRI (fMRI) helps to visualize regional brain activity. It
provides a reliable way to lateralize language dominance and eliminates
the need for invasive intracarotid amobarbital test in 80% or more
patients.
Magnetoencephalography
(MEG) is a noninvasive type of imaging based on the brain's ability to
produce small magnetic dipoles with neuronal discharges. Large groups of
neurons fire synchronously, as in an interictal epileptiform discharge
and can be sensed with sophisticated imaging equipment and complicated
computer analysis. This map of the epileptiform discharge can be useful
for diagnostic purposes and for presurgical planning of intracranial
electrode placement. However, MEG is still in the development
stage.
Neurophysiological assessment:
The
most useful test in epilepsy diagnosis is the electroencephalography
(EEG). By definition, epileptiform discharges are interictal patterns
that include spikes, spike-and-slow-wave complexes, sharp waves, and
sharp-and-slow-wave complexes. More than one seizure focus or psychogenic
or physiologic nonepileptic seizure may be found when numerous episodes
are recorded. Hence all surgical candidates should undergo
long-term video EEG monitoring preoperatively to record several
typical seizures.
Traditionally,
EEG is recorded extra cranially with scalp electrodes; they only monitor
from the superior and lateral cortex of the hemispheres. The frequency of
the initial ictal discharge in the scalp EEG correlates with the degree
of hippocampal pathology in temporal lobe epilepsy. Seizures originating from the mesial surface
of the cerebral cortex may be difficult to detect by simple scalp telemetry
and, therefore, a negative result does not necessarily exclude surgery.
In certain patients, who may be candidates for functional procedures, the
interictal EEG may be an important selection criterion, as with bilateral
synchronous spike wave discharges for callosotomy and “electrical status
epilepticus of slow sleep” (ESESS) in Landau - Kleffner syndrome (LKS).
Excellent surgical results have been reported in patients
with unilateral preponderance of interictal epileptiform discharges of
3:1, along with ipsilateral ictal onset on ictal EEG.
Neuropsychological
assessment:
Epilepsy is often associated with psychiatric disorders such as
behavioral changes, major mood disorders or psychosis. Neuropsychology
provides information about size, location and degree of epileptic
dysfunction. Preoperative evaluation assists in predicting epilepsy
surgery outcome and thus helps in selecting ideal candidates for surgery.
Basic neuropsychological tests have been used for many years to
assess verbal and non-verbal intelligence and memory. These tests may
help to evaluate the potential effect of resective surgery on brain
function. Neuropsychological testing can also be used for nonoperative or
postoperative epilepsy patients to assess their level of cognitive
functioning in order to assist with vocational and cognitive
rehabilitation in the context of their neurological disorder.
Invasive
assessment:
The
use of invasive techniques has been much reduced by improved understanding
of the pathology of epilepsy and the development of modern brain imaging.
If the data gathered from the clinical examination, imaging studies and
noninvasive EEG evaluation are conflicting or disparities arise in the
presumed localization of the seizure, invasive monitoring is
warranted.
Carotid
amobarbital (Wada) test:
The
intracarotid amobarbital test was developed by Jun Wada to preoperatively
determine which hemisphere contains language function. The standard test
involves injection of sodium amobarbital into each internal carotid
artery. The primary use of the Wada test is to assess language
lateralization and the ability of the contralateral mesial temporal
structures to support memory postoperatively when anteromedial temporal
resection (AMTR) is being considered to treat medically intractable
epilepsy. The intracarotid amobarbital
test can also be used to demonstrate bilateral secondary synchrony in
which an epileptic focus in one hemisphere is thought to be driving
activity in the other hemisphere. Alternatively methohexital and
propofol can be used when amobarbital is not available.
Invasive
Electrodes (Table 2):
Invasive
neurophysiology is indicated when there is a lack of concordance between
investigations or observations and when there is a discrepancy between
the interictal neurophysiological findings and the suspected seizure
origin. Invasive electrode placements may be used with videotelemetry to
clarify the nature and origin of a patient’s seizures. The depth
electrodes are placed stereotactically while other
cranial electrodes require craniotomy.
The interpretation of data obtained from intracranial recordings needs a
sophisticated technological set-up with video-EEG and an experienced
neurophysiologist. The use of depth electrodes has decreased with the
advent of good MRI and varies considerably between centers, dependent
upon their cases, other facilities and previous experience.
|
(Table 2) Invasive electrodes.
|
|
Cranial electrodes
|
Indication
|
|
|
· Extradural electrodes
|
Used in sampling
wide areas with minimal invasion
|
|
|
· Subdural strip and grid
electrodes
|
Used in temporal /
extratemporal (well confined cortex).
With free hand
placement, subdural grid electrodes may be used for functional mapping
extraoperatively, in advance of the cortical excision, by passing small
currents between implanted electrodes.
|
|
|
· Cortical plates / grids
|
Used in
extratemporal cortex (large areas i.e. out of the multiple areas which
area is the source of seizure)
Extraoperative
cortical mapping and stimulation
|
|
|
· Depth electrodes
|
Used
in seizures arising from hippocampus/amygdale; Stereotactically
determined placement of multicontact wire electrodes may be used
primarily to explore an area of brain, surface and depth in order to
delineate the epileptogenic zone and may include some stimulation
protocols for functional localization and to provoke seizures.
|
|
|
· Foramen ovale electrodes
(Percutaneous placement similar to trigeminal glycerol block.)
|
Placed through
foramen ovale to lie close to mesial surface of temporal lobe can
provide lateralization, to distinguish temporal from extratemporal
onset of seizures and mesial temporal from lateral temporal onset.
|
|
|
· Sphenoidal electrodes
(Multi-standard wires are inserted below the zygomatic
arch to the region of foremen ovale).
|
Used especially for
temporal lobe focus
|
|
Intraoperative
electrocorticography (ECoG):
Intraoperative
ECoG is an interictal recording. It provides a possibility to delineate
an epileptogenic region intraoperatively and is a useful tool in
extratemporal resecting procedures. A hand held stimulator allows
for precise individual localization of sensory, motor and language areas;
it has limitations for sufficiently delineating the epileptogenic zone or
eloquent cortices and cannot be used preoperatively for risk assessment,
therapeutic decision-making and surgical planning.
Surgical
Pathology:
In
many situations, the extent and nature of the cerebral pathology
determine both the possible surgical intervention and the outcome of
surgery. Table 3 provides a list of surgical pathologies observed in
these epileptic patients.
|
Temporal lobe
epilepsy:
It
is the most frequent form of adult refractory epilepsy and also
presents the best prognosis after surgical treatment. 80% of patients
with temporal epilepsy present with clinical, electrophysiological, and
imaging signs and symptoms suggestive of mesial temporal sclerosis
(MTS). MTS typically causes complex partial seizures in young adult
patients with a history of prolonged febrile seizures during childhood.
However, despite intensive investigations, it has not been determined
whether MTS is the cause or the result of prolonged seizures. 5-30% of
TLE patients were shown to harbor associated pathology in one study.
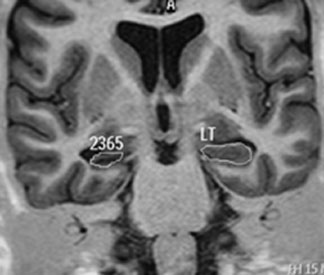
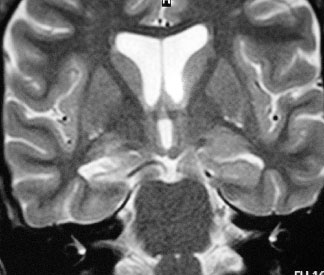
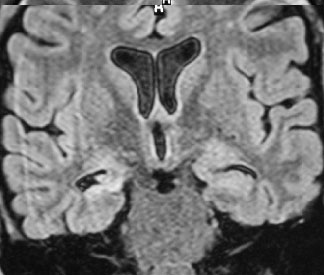
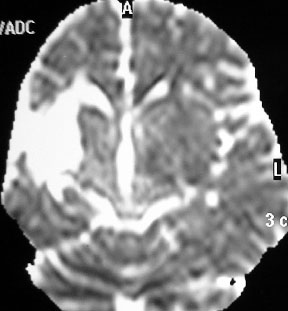
MTS
(Fig 1) is characterized by atrophy of this structure in the
T1-weighted sequence or in the volumetric reconstructions and by an
increase of the signal in T2-weighted and the fluid-attenuated
inversion recovery sequence. EEG demonstrate the presence of rhythmic
activities in the mesial electrodes of the interictal EEG. SPECT
reveals local metabolic changes.
Extratemporal
Epilepsies:
Extratemporal
epilepsies may be lesional or non lesional. Identifiable
structural lesions carry a better surgical prognosis and they commonly
include tumors, vascular lesions, and cortical abnormalities. They are
discussed in respective chapters. Nonlesional epilepsy represent the
greatest challenge for the surgical treatment of epilepsies, with a
lower success rate ranging from 20 to 55% of the patients.
Invasive monitoring is of fundamental importance in these patients.
Extratemporal
epilepsies tend to spread rapidly especially those involving the
frontal lobe, the seizures rapidly cross to the contralateral side,
also impairing their lateralization. Most patients with extratemporal
epilepsies present extensive irritative multilobar surface areas in
their EEG monitoring. Invasive monitoring with deep or subdural
electrodes is necessary especially when the structural lesion cannot be
located. Intraoperative eletrocorticography is considered to
be an indispensable technique for defining the irritative zone in
patients with refractory extratemporal epilepsies.
|
|
|
|
(Fig 1a) Rt. MTS – Coronal MRI T1
|
|
|
|
(Fig 1b) Rt. MTS – Coronal MRI T2
|
|
|
(Fig 1c) Rt. MTS – Coronal MRI FLAIR
|
|
(Table 3) Pathological lesions associated with
intractable epilepsies
|
|
Type
|
Lesions
|
Remarks
|
|
Congenital lesions
|
Congenital
malformations of cortical development such as cortical dysplasias,
heterotopia, schizencephalic clefts and the various forms of
phakomatoses (such as Sturge Weber syndrome)
Hemispheric lesions
such as
infantile
hemiplegia syndrome, hemimegalencephaly, dysplastic hemisphere,
and Rasmussen (progressive chronic encephalitis) encephalitis.
|
Seizure outcome
after resection of such malformations is variable and directly relates
to the focal extent of the lesion.
Removal of the
hemisphere or multilobar resection may be considered for controlling
seizures.
|
|
Atrophic
lesion
|
Mesial temporal
sclerosis
|
Anteromedial
temporal resection yields best results.
|
|
Vascular lesions
|
Infarction
AVMs
Cavernomas
Hemorrhage
|
Excision
of the vascular abnormality and surrounding hemosiderin-stained cortex;
simple lesionectomy often fails to stop the seizures
|
|
Neoplasm like
|
DNET
Hypothalamic
hamartomas
ganglio-glioma,
gangliocytoma and pilocytic and fibrillary astrocytoma
|
Removal
of gross tumor, and the immediate surrounding tissue if possible will
give the optimium result.
|
|
Miscellaneous
|
Arachnoid cyst
Traumatic
encephalomalacia
|
Excision
|
Surgical
procedures (Table
4):
Lesions
such as cavernous angiomas, low grade astrocytomas, cortical dysplasias
and areas of focal atrophy that are clearly the cause of their seizures
are often detected by MRI nowadays. Removal of the lesion with a small
rim of surrounding cortex is often successful in controlling seizures. Lesionectomy
is associated with excellent results with success rates that are
generally better than with surgery performed in patients without discrete
lesions. Behavioral problems in patients with uncontrolled temporal lobe
epilepsy are well documented and they will often improve or disappear if
seizure control is good. Psychosis supervening upon chronic epilepsy is
usually a late event. Hence, early surgical intervention is favorable.
|
(Table 4) Surgical procedures
|
|
Resective surgery
|
Non resective (disconnective) surgery
|
|
Temporal
resection
Extratemporal
resection
Multilobar
resection
Hemispherectomy
Hemispherotomy
|
Callosotomy
Multiple
subpial transections
Stereotactic
lesioning
Deep
brain stimulation
Cerebellar
stimulation
Vagal
nerve stimulation
Radiosurgery
|
Resective
surgery:
These
operations are performed when a well localized epileptic focus is
identified in a part of the brain that can be safely removed without an
unacceptable neurological deficit. Established measures to reliably
assess the eloquence of certain cortex areas are cortical mapping through
chronically implanted electrodes and intraoperative mapping during awake
craniotomy.
Resective
procedures are more effective and have a higher success rate 75 – 83 %.
The application of resective techniques varies in extent and site and it
is probably best to classify procedures into three groups: temporal
resections, extratemporal resections and major resections. Extra-temporal
resections are much less commonly performed with the majority being
carried out in the frontal lobe.
Temporal
Resections:
AMTR
with amygdalo-hippocampectomy is a modification of the classical temporal
lobectomy by reducing the amount of cortical removal and extending the
hippocampal resection. It is the most commonly performed surgery with
well defined indications and best results. Complex partial seizures with
semiology typical of mesial temporal lobe epilepsy and with
EEG confirmation that seizures begin over the temporal area and MRI
evidence of unilateral hippocampal atrophy or unilateral temporal lobe
hypometabolism on PET scans respond best to AMTR. The
mechanism of chronic temporal lobe epilepsy probably differs from focal
epilepsy in other parts of the brain and this is important in assessing
the value of various procedures. In temporal lobe epilepsy associated
with mesial temporal sclerosis, there is good evidence for the
“amplifier” mechanism which states that a normal parahippocampal gyrus is
part of the neurophysiological circuit responsible for the persistence of
the epilepsy and will need to be removed to obtain a cure.
The
extent and technique of temporal lobe resection vary between different
epilepsy centers and surgeons. The standardized technique is en bloc
removal of the anterior temporal lobe along with a part of hippocampus,
uncus and dorso lateral parts of amygdale. In the dominant hemisphere,
the majority of the superior temporal gyrus must be preserved. The
insular cortex must remain undisturbed if the risk of a manipulation
hemiplegia is to be avoided. The posterior extent of the resection is
governed by the risk of hemianopia. In adults, the limit is
around 6.5 cm; in smaller children, it is convenient to use the height of
the temporal lobe at the mid-Sylvian point as the posterior extent of the
resection.
It
is also possible to carry out a restricted removal of the mesial temporal
structures, described as selective amygdalohippocampectomy. Sometimes
just the hippocampus part of the structure is removed. The purpose is to
save as much lateral neocortex as possible to minimize memory function.
Direct
operative mortality following temporal lobe resection is rare. Possible
complications with ATMR include homonymous superior quadrantanopsia due
to involvement of either optic tract or radiation, language deficits and
manipulation hemiplegia due to vascular injury or spasm involving the
sylvian vessels, anterior choroidal artery branches supplying the
cerebral peduncle or the perforators supplying the internal capsule.
Recurrent seizures are more likely following temporal lobectomy when the
hippocampus is not removed. Temporal lobe surgery can produce a
schizophreniform psychosis, often associated with left-sided resections,
but this is rare, less than 1% in one study.
Extra-temporal
Resections:
Extra-temporal
resections account for less than 20 % of epilepsy surgeries. The
surgical outcome is generally poor when compared to that of temporal
lobe. Rapid seizure spread complicating electrophysiologic localization,
and more frequent overlap with eloquent areas imposing limits on optimal
resection of the epileptogenic zone may be the reasons for poor outcome.
The Montreal Neurological Institute has reported in their last
review of 257 patients with non-tumoral lesions, 26% had complete freedom
from seizures and a further 30% had a marked reduction in seizures. The
extent of the extratemporal resection is based upon the pathology rather
than the neurophysiological abnormalities. It is recommended to resect a
small rim of adjoining cortex as well.
Most
extratemporal resections involve frontal lobe. Resection from the
parietal and occipital region is rare. When there is a pre-existing
deficit, then there is less likelihood of an increase as a result of
operation and, therefore, it is more reasonable to attempt it. Occipital
lobe invariably involves the temporal lobe, often bilaterally, and
temporal lobe seizures themselves can have visual components in their
clinical presentation.
Hemispheric
procedures:
Hemispheric
procedures in the second or third year of life do not carry any risk of
increased deficit and hence ideal for patients who come at early stages
for diagnosis and evaluation. They are usefull for intractable epilepsy
associated with major lesions involving one hemisphere, such as the
hemiconvulsion – hemiplegia - epilepsy syndrome (HHE syndrome), Sturge -
Weber syndrome, Rasmussen’s encephalitis and hemimegalencephaly. They
include multilobar resections, hemispherectomy and hemispherotomy.
Multilobar
resection is used to remove an epileptogenic area or pathology, which
does not involve the whole hemisphere and by means of which useful cortex
may be spared. This technique is used for patients with widespread
cortical neuronal migration disorder and gross destructive lesions
consequent upon trauma or cerebral infarction. Recovery from seizures or
significant improvement has been reported in 53% of patients treated.
|
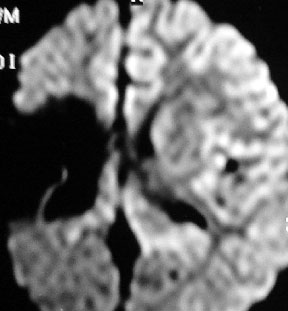
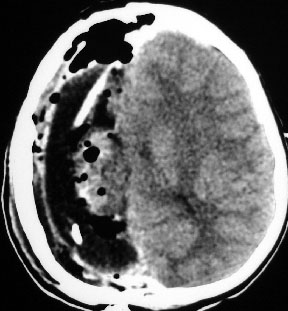
(Fig 2) Hemispherectomy for infantile hemiplgia
|
|
|
|
|
Infantile MCA infarct with seizures in 12 years
old boy – diffusion MRI
|
Infantile MCA infarct with seizures in 12 years
old boy – diffusion axial MRI T2
|
|

|
|
|
Infantile MCA infarct with seizures in 12 years
old boy – coronal MRI
|
Post hemispherectomy CT
|
Hemispherectomy
was originally advocated for infantile hemiplegia (Fig 2) epilepsy and
behavior disorder. This was abandoned in the 1970s because of
the complication of cerebral hemosiderosis which occurred in up to a
third of patients and was often fatal. Subsequent modifications have been
described. 'Hemidecortication' described by Benjamin et al, consists
of removal of the whole cerebral cortex, with sparing of the white
matter, thus avoiding opening of the lateral ventricle. The 'modified
hemispherectomy' as described by Adams consists of an
anatomic hemispherectomy followed by occlusion of the ipsilateral foramen
of Monro with muscle to prevent communication between ventricular CSF and
the hemispherectomy cavity. The use of Adams’ modification in which,
amongst other features, the enormous cavity in contact with the
subarachnoid space is converted into an extradural space led to a
significant reduction of delayed hemosiderosis.
Hemispherotomy has replaced the more invasive hemispherectomy. In
hemispherotomy, cortex is disconnected from all subcortical structures
and the interhemispheric commissures are divided, but the brain remains
in place. The technique involves shorter operation times, much less
operative trauma and less blood loss. Other benefits include
improved intellectual performance and behavior if the seizures are
controlled. A vertical parasaggital approach described by Delalande,
a peri-insular technique described by Villemure and
later more modifications have been described. Rasmussen has
reported over 85% marked improvement and about 60% seizure free
outcome.
Non resective / disconnective procedures:
These
operations modify the brain function so as to improve the control of
epilepsy. The aim is to isolate or disconnect the epileptogenic area of
the ipsilateral hemisphere or to prevent the propagation of the seizure
to the contralateral hemisphere.
Originally epilepsy surgery was based on physiological as well as
structural principles. Increasing knowledge of the underlying pathology
and improved direct brain imaging have resulted in less attention being
paid to functional operations, especially stereotactic lesioning.
Currently, the available procedures for epilepsy are stereotactic
lesioning, cutting various fiber tracts or other connections, including
the various methods of callosotomy and multiple sub-pial transection,
and, finally, brain stimulation either with intracranial electrodes or
vagal nerve stimulation. These procedures are not standardized and have a
lower success rate.
Callostomy:
Corpus callostomy prevents the bilateral synchrony of a cortical
epileptiform activity that may result in seizures with bilateral motor
manifestations. This procedure was based upon observations in
experimental models of epilepsy and a fortuitous observation that
seizures improved in a patient whose glioma had invaded the anterior
corpus callosum.
Callostomy
disrupts one or more major CNS pathways used in seizure generalization
and decreases the frequency and severity of either primary or secondary
generalized seizures. It is indicated when the patient has a severely
damaged hemisphere but motor, sensory or visual function that would be
valuable to preserve. It helps in patients with generalized tonic-clonic,
tonic or myoclonic seizures or seizures with drop attacks refractory to
medical treatment. It is particularly indicated in atonic or drop attacks
and in patients who are prone to violent falls that often result in head
injury. They tend to improve markedly although a complete cure of seizures
is extremely rare. In many patients subjected to callosotomy,
there is no demonstrable structural lesion and, in these patients, the
only absolute indication for callosal section seems to be bilateral
synchronous EEG discharges.
It
is valuable to assess the degree of section post-operatively, using the
MRI. Generally, complete callosotomy has been abandoned and an anterior
two-thirds section substituted; although a complete callosal section
yields best results the risk of disconnection is greatest. It is
recommended that the splenium is spared.
The
goal is to reduce seizure frequency and associated morbidity and not a
seizure free outcome. The seizure disorder usually persists
postoperatively but seizures may become less frequent, less disabling,
and less violent. Partial seizures and myoclonic jerks may not
respond and may even be made worse by the procedure.
Two
cognitive complications may follow callosal section. Speech may be
affected in patients of mixed cerebral dominance, where inter-hemispheric
communication is essential for the proper comprehension and production of
speech and related functions. The second complication is the posterior
disconnection syndrome, in which complex tasks requiring the utilization
of information from both hemispheres become impossible. It is associated
with division of the posterior fibers at a one-stage callosotomy and may
be less severe when the operation is staged. Complete section of the
corpus callosum is reserved for patients whose response to anterior section
is unsatisfactory. Reports suggest 50-80% reduction in the seizure
frequency.
Multiple
Subpial Transsection (MST):
First
described by Morrell and Whisler, MST is the only acceptable surgical
treatment if the epileptogenic focus involves eloquent cortex. MST
depends upon the observation that cortical organization is columnar. The
functions of eloquent cortex are subserved by vertical columns, whereas
the propagation of epileptic impulses occurs through horizontal fiber
connections. Morrell reasoned that if multiple transsections
of the cortex were made below the pia, preserving the cortical vessels,
it would reduce epileptiform activity whilst preserving essential
function.
MST
involves selective division, with specially constructed hooks under
microscopic control, of the horizontal sub pial fibres at 5-mm intervals
along the gyri which exhibit epileptiform activity. It is important to
maintain the integrity of the pia and avoid cortical blood vessels and
also to be careful of vessels in the depths of the sulcus; the buried
cortex of the insula is especially vulnerable. Both Morrell and other
authors describe using this technique both alone and in combination with
resection.
Most
patients present temporary deficits during the postoperative period, with
improvement within 2–4 weeks and a return to the previous functional
status. The incidence of permanent deficits is about 5%. Some
neurological deficits appear postoperatively but these generally resolve
over several weeks with satisfactory improvement in seizure control in 70
% of patients. The effect on seizure control is variable; most
series report reduction rather than abolition of seizures by MST
alone.
MSTs
can be used for the treatment of continuous partial epilepsy; focal
seizures of the sensory, somatosensory,or visual cortex; resection with
evidence of epileptiform activity in the adjacent eloquent areas It
is also very successful in Landau - Kleffner syndrome and has also been
proposed to deal with patients with widespread multi-focal epilepsy.
Stereotactic
Lesioning:
Stereotactic
amygdalotomy, hippocampotomy and fornicotomy have been described in the
literature; however, outcome with modern stereotactic ablative surgery
using current image guided technology is not as favorable as those
obtained with standard temporal resections.
Stimulation
(augmentive) procedures:
This
became practical with the miniaturization of electronic components and
development of safe silicone polymers. Cooper applied stimulation to the
surface of the cerebellum on the basis of animal studies in which
cortical discharges were reduced or inhibited by cerebellar electrical
stimulation. But subsequent studies showed this treatment to be
ineffective and it fell into disuse. Numerous attempts have been made to
reduce seizure frequency by stimulation of deep brain
structures, including the anterior thalamus, the centromedian
thalamic nucleus, the caudate nucleus, the posterior
hypothalamus, and the hippocampus. Theories relating to
centrencephalic epilepsy and a thalamo cortical relay had suggested that
chronic thalamic stimulation might lead to better control of the
epilepsy.
Similar
physiological considerations lead to intermittent retrograde stimulation
of the left vagus nerve. Its mechanism of action is uncertain, but it is
known to desynchronize the electroencephalogram.14 Vagus
nerve stimulation is recommended in those with medically refractory
epilepsy who are not candidates for epilepsy surgery and in those where
the surgery has failed, although the results of a number of uncontrolled
trials. There are inevitable minor side effects associated with this
stimulation, including hoarseness and a sensation in the throat, and
there is also the risk of electrode movement, cable fracture and receiver
or generator failure.
Radiosurgery:
Stereotactic-guided
radiotherapy for epilepsy has been described, using either a linear
accelerator or the Leksell Gamma Knife. There is considerable experience
using this method of treatment for obliteration of other lesions in the
brain. It has come to the fore in the treatment of mesial temporal
sclerosis and the largest experience has been reported by Regis et al
Their report showed that, at 2 years, 81% of 16 patients were seizure
free. Good results have also been reported with hypothalamic hamartomas,
AVMs and cavernomas.
Outcome:
Surgical
resection of the epileptogenic area can be curative or can provide
significant amelioration of the seizure frequency in majority of
individuals. AMTR yields a better quality of life and reduced depression
and anxiety as soon as 3 months after surgery, compared with continued
medical therapy. Epilepsy duration is the most important predictor for
long-term surgical outcome. Presence of unilateral temporal interictal
epileptiform activity, unilateral temporal ictal onset, presurgery
seizure frequency below 20 complex partial seizures per month, presence
of febrile seizures are other factors associated with better outcome.
A highly localized interictal scalp EEG focus as a
predictor of outcome.
Surgical
resection of a unilateral atrophic hippocampus renders more than 80% of
patients seizure free while bilateral atrophy or lack of atrophy is found
to be less favourable. Patients with brain damage2
and mentally retarded patients are less likely to improve. Outcome after
surgery for lesional epilepsy is variable ranging in literature from 39
to 83%. Incomplete removal of the epileptic focus being the main reason
for poor surgical outcome.
Functional
procedures are not standardized and only relieve epilepsy completely in
less than 5% of cases, although they will produce significant and useful
amelioration of the fits. The long-term psychosocial effects of epilepsy
surgery are still unclear.
In
children, data suggest however that although there are predictive factors
with regard to seizure freedom, reduction or withdrawal of
anticonvulsants cannot be guaranteed, with lower rates of
seizure freedom for developmental malformations, particularly
hemimegalancephaly. Early data from children undergoing temporal
lobectomy suggested little overall risk to cognitive function with recent data suggesting greater likelihood
of improvement in children than adults 12 months following surgery when
compared to preoperatively. Similar result is seen following
hemidisconnection procedures, most studies report little longitudinal
change in IQ Children with developmental pathology had a significantly
lower IQ presurgery, with no significant gain post surgery.
Most
patients will require ongoing anticonvulsant treatment for two or more
years. Mortality and major morbidity after surgery for epilepsy are
nowadays low: mortality is less than 0.5% and hemiparesis and hemianopia
occur in less than 2% of cases.
There
has been interest in the psychosocial results of epilepsy surgery since
the 1950s. Guldvog examined two groups of patients treated
medically and surgically and followed them for 20 years. Significant
improvement in the work situation was seen only in those who were in
full-time education or work before surgery. Similar findings were
reported by McLachlan in which patients treated both
medically and surgically had improvement in quality of life if they were
seizure free or had a 90% reduction at 2 years. The surgical group was
more likely to attain this target.
There
is no consensus on withdrawal of drugs but patients following surgery are
continued on the preoperative anticonvulsant for at least 1 year. At the
end of 1 year an EEG is taken and if normal the drug is gradually
tapered. Effects on overall health status, quality of life and financial
benefits to the state or community of epilepsy surgery have not been
adequately studied.
Re-operation:
The
most reported causes of treatment failure were dual pathology, recurrent
tumor, limited resection to preserve function, widespread developmental
abnormalities, and electrographic sampling error.90 The
most reported common cause for poor outcome of the original operation in
patients with temporal lobe epilepsy was insufficient hippocampal
resection.
Patients
who were most likely to benefit from reoperation are: 1) those with
initially incompletely resected structural lesions; 2) those who were
initially evaluated with invasive ictal monitoring; and 3) those who
underwent further resection of the initial operative site rather than
resection of a different cortical region.115 Patients with
initial focal resections followed by enlargement of the original
operative site have the most successful outcome, especially those with
complex partial seizures of temporal lobe origin.
In
a series of reoperation,41 44.3% were seizure free, 30.5%
significantly improved and 25.2% were not improved. Temporal lobe
resections tended to do better, with 55.7% seizure free and 16.5% not
improved, whereas for other resections, only 24.5% were seizure free and
40% were not improved. When there is a structural lesion which has been
missed or incompletely removed, then the seizure-free proportion rises to
80 - 90%.
|
Key points
|
|
·
Epilepsy surgery
is safer and less invasive and more effective with better seizure
control rates with lower morbidity and mortality rates.
·
A presurgical,
video EEG to define and localize the seizure focus, MRI and
localization of eloquent cortex by neuropsychological or functional
testing are mandatory..
·
If no lesion is
seen in MRI, SPECT and PET may be useful; intraictal SPECT scanning of
regional blood-flow changes is an extremely useful tool for
confirmation of a seizure focus and PET is helpful to correlate abnormal
glucose metabolism with areas of anatomical abnormality.
·
If SPECT and PET
are inconclusive, invasive electrodes help; electrocorticography can
further define the boundary between functional and non-functional
cortex.
·
Anterior temporal
lobectomy with hippocampectomy is the most commonly performed surgical
procedure; early surgery has a better outcome.
·
Excision of areas
of cortical dysplasia are been performed more frequently in recent
years, as this condition can now usually be defined with MRI; other
resective surgery includes multilobar resection and hemispherectomy.
·
Corpus callostomy
and MST are palliative procedures that may benefit some patients with
severe generalized seizure patterns.
|
|