|
The
jugular foramen (JF) lesions, once thought to be one of the most
difficult surgically unapproachable ones, are now becoming safely
manageable with reasonable morbidity and mortality rates. This
recent achievement has been accomplished by the extraordinary efforts put
forth in the understanding of the microsurgical techniques and
instrumentations and by the most exciting and promising innovations in
cranial base surgery. Added to this revolutionary neuro-surgical armamentarium,
the parallel advances in the field of neuroradiology,
neuroanesthesiology, neuroelectrophysiology and neuro-intensive care, in
fact, paved the way for the successful management of these lesions as
seen today. But the highly complex nature of the jugular foramen
and even more perplexing morphological organization of its surrounding
neurovascular structures coupled with the plethora of pathological
conditions encountered in this region still pose a major challenge to the
neurosurgeon. From the pre-microsurgical era to the microsurgical
era various safe approaches have been established. A proper patient
selection, a thorough pre-operative work-up, choosing the ideal surgical
approach, and the interdisciplinary team work involving neurosurgeon,
otologist, neuroradiologist and plastic surgeon, has made the now
preferred single stage procedure feasible in dealing with these
bewildering lesions.
In
this article, we review the salient anatomical, pathological radiological
and clinical features of JF lesions and indications, these discuss the
techniques, merits, demerits and the complications of the major
approaches to the JF based on our experience of 9 cases.
ANATOMICAL CONSIDERATIONS:
Since the neural,
arterial, venous, muscular and osseous relationships are exhaustive, only
the salient features related to jugular foramen and mentioned here.
The jugular foramen is located at the posterolateral skull base with its
long axis obliquely directed from posterolateral to anteromedial
direction and is formed by the petrous temporal bone anterolaterally and
by the jugular process of condylar part of the occipital bone
postermedially. It is configured around the sigmoid sinus and the
inferior petrosal sinus. The junction where the transverse sinus
continues as the sigmoid sinus is indicated externally by the asterion at
which point the vein of Labbe enters the sinuses.
The right
foramen is larger than the left in 68%, equal in 12% and smaller than the
left in 20%, possibly due to the difference in the size of the sigmoid
sinus and the jugular bulb. On the intracranial side the jugular
foramen is related inferior to the porus acoustics and superolateral to
the intracranial orifice of the hypoglossal canal. On the
extracranial side it is Iocated just behind the carotid cannal separated
by the carotid ridge, lateral to anterior half of the occipital condyle,
antermedial to the stylomastoid foramen and posteromedial to the styloid
process.
The jugular
foramen is traditionally divided into a large posterolateral compartment
(pars venosa) and a smaller anteromedial compartment (pars
nervosa). This view has been recently challenged by Katsura et al
who has divided the jugular foramen into three compartments : two venous
compartments and one neural intrajugular compartment in between.
The venous compartments include a large posterolateral sigmoid part and a
small anteromedial petrosal part. At the junction of these two
compartments there are two bony prominences (intrajugular processes)
arising from the temporal and occipital bones joined by a fibrous or less
commonly osseous bridge forming the intrajugular septum.
The dura
over the intrajugular septum has two characteristic performations : the
glosso-pharyngeal meatus for IX nerve and larger vagal meatus for X and
XI nerves. Both of the meati are located on the medial side of the
intrajugular processes and septum, being consistently separted by a dural
septum. Over the upper and lateral margin of the intrajugular part
of the jugular foramen the dura is thickened forming a roof or lip that
projects inferiorly and medially to partially cover the IX and X nerves
meati. This thick dural fold is called plica occipitals oblique or
jugular dural fold. The lip projects most prominently over the IX
nerve meatus whereas the lip over the X nerve is less prominent.
The
inferior petrosal sinus (IPS) joins the jugular bulb in 90%, passing
between IX nerve superolaterally and X and XI nerves
inferomedially. In 10% it drains directly into the internal jugular
vein. The occipital condyle (OC) contains condylar emissary vein in
70% of cases. This posterior condylar vein enters the jugular
foramen at its posteromedial part and serves as a landmark to the foramen
for the posterior approaches. The hypoglossal canal contains a
venous plexus, called anterior condylar vein in addition to XII
nerve. The IX nerve enters the jugular foramen just below the
cochlear aqueduct piercing the dura at the pyramid fossa, expands at the
site of the superior and inferior ganglia and courses forwards along the
medial side of the intrajugular ridge before turning downward. The
X nerve enters jugular foramen below the IX nerve. Its superior
ganglion is located at the level of dural roof of the JF and the inferior
ganglion is located below the JF at the level of atlanto-occipital (AO)
joint. The X nerve after piercing the dura quickly turns downwards
without having the forward course within the JF. The XI nerve
bundle blends into lower margin of X nerve at the level of JF.
The
relationships between lower cranial nerves (LX-XII) and the major vessels
(internal) carotid artery (ICA), internal jugular vein (IJV), external
carotid artery (ECA) and branches of vertebral artery (VA) are extremely
complex at the level of JF and in the upper neck. At the level of
the skull base the IJV courses just posterior to the ICA being separated
by the carotid ridge. At this level both the artery and the vein
are surrounded by a thick fibrous attachment of the carotid sheath to the
periosteum of the skull base. The styloid process with the muscles
attached to it separates the ECA laterally from ICA medially. The
IX, X, XI and XII nerves at the exit from their respective foramina,
first lie medially to both the ICA and the IJV with IX being most lateral
and XII most medial; then IX, XI and XII nerves pass laterally between
ICA and IJV; later the IX and XII descend forward along the lateral
surface of ICA while XI descends backward along the lateral surface of
IJV. The posterior branches of ECA (occipital and ascending
pharyngeal) supply the meninges around the Jf and are the main feeding
arteries of the JF lesions. The vertebral branches that are
encountered near the JF region include the meningeal and posterior spinal
arteries and posterior inferior cerebellar artery (PICA) having close
relationship with IJV, which lies just anterior to the transverse process
of the atlas.
PATHOLOGY:
The
jugular foramen lesions are rare in clinical practice. Owing to the
presence of osseous, muscular, neural, vascular, dura and connective
issue elements in the jugular foramen region lesions arising from these
elements are encountered in this region, some are more common then
others. They are broadly classified into intrinsic and extrinsic or
neoplastic and nonneoplastic. Table I lists the lesions involving
the jugular foramen region. Since the choice of the surgical
approaches is dependent on the site of the origin, size and extent of the
lesion, attempts were made to classify these lesions into various types
or classes, for example Fisch’s and Glasscock and Jacobson’s
classification for glomus jugular tumours and Keye’s and Franklin’s
classification for schwannoma.
The
one proposed by Bertalanffy and Ulrich Sure is applicable to any type of
lesion, which is as follows :
Type
I -
Small lesions confined to jugular foramen
Type
II -
Intrinsic lesions of lower brainstem located in the vicinity of the
jugular foramen
Type
III
- Lesions of jugular foramen with predominant intradural
extension located above the level of foramen magnum
Type
IV - Lesions
of Jugular foramen with intradural extension beyond the level of foramen
magnum into the spinal canal.
Type
V -
Lesions of Jugular foramen with intra and extradural extension into the
petrous bone.
Type
VI
- Lesions of Jugular foramen with predominant extradural
extension.
Neoplastic:
Paraganglioma ,Schwannoma, Meningioma & Metastisis
(hematogenous, nasopharyngeal ca) are the common
ones.
Exophytic
brainstem glioma, Choroid plexus papilloma,
Hemangioblastoma, Hemangiopericytoma, Chordoma, Chondroma,
Chondroblastoma, Chondrosarcoma, Chondromyxoid fibroma, Osteoblastoma,
Plastacytoma, cavernoma, Rhabdomyosarcoma, Ca of tympanic cavity and
neuroeneteric cyst are uncommon.
Non
neoplastic:
Internal jugular vein thrombosis, Large jugular bulb pseudomass(included
because of radiological importance) are the common non-neoplastic jugular
foramen lesions.
Aneurysm,Osteomyelitis,
Malignant external otitis,Cholesterol granuloma, and Amyloidoma are
uncommon.
CLINICAL
MANIFESTATIONS:
The
clinical presentation of jugular foramen lesions is dependent on size,
extent and pathology of the tumour. Typically they produce the
jugular foramen syndrome (Vernet’s syndrome) and depending on their
extension produce other related syndrome (Table 2). The patients
with IX, X and XI cranial nerves dysfunction may present with dysphagia,
dysarthria, hoarseness of voice, dystphonia, nasal regurgitation,
ipsilateral trapezius and sternomastoid muscle weakness and atrophy,
depressed gag reflex, palatal droop on affected side with ipsilateral
vocal cord paralysis and loss of taste on the posterior 1/3rd
of the tongue, paresis of soft palate, uvula, pharynx and larynx.
Some patients may present with neuralgic pain in IX and X nerves
distribution. Because of slow expansile growth of these lesions,
the lower cranial nerves dysfunction is of gradual onset and in most
patients, they are well tolerated as a result of gradual
compensation. As a result, though imaging studies reveal extensive
involvement of these neural structures, patients may have only subtle
manifestation of their dysfunction. Even though a positive
correlation exists between cranial nerve palsy and tumour invasion, lack
of preoperative nerves dysfunction does not correlate with degree of
nerve invasion found at the time of surgery (15). The anterior
extension encasing cavernous sinus and internal carotide artery may
produce Horner’s syndrome and III, IV, V and VI nerves palsy.
Intracranial extension can produce posterior fossa symptoms as nystagmus,
ataxia, hemiparesis and increased intracranial tension (16). The
extracranial extension along the internal jugular vein can produce a
visible mass in the oropharynx or a palpable mass in the neck. The
intraluminal growth can block venous drainage and occlude the sigmoid
sinus and if present bilaterally, increased intracranial tension can occur.
The intracranial extension superiorly can produce the cerebollopontine
angle syndrome (deafness, tinnitus, VII nerve palsy) and those extending
still laterally can produce bloody otorrhoea, a visible mass through
tympanic membrane and a bruit over the mastoid.
THE
JUGULAR FORAMEN AND RELATED SYNDROMES:
|
SYNDROME
|
CRANIAL NERVES
|
SITE OF INVOLVEMENT
|
|
Vernet’s
Syndrome
|
IX, X XI
|
Lesions
in jugular foramen
|
|
Collect-Sicard
Syndrome
|
IX, X, XI, XII
|
Lesions in retroparotid
space
|
|
Vallaret’s Syndrome
|
IX, X, XI, XII
Sympatheic
chain
|
Retropharyngeal
extension
|
|
Schmidt’s
Syndrome
|
occasionally VII,
|
Intradural extension
|
|
Avellis Syndrome
|
X, XI
XI
(accessory to X)
|
Intradural extension
|
|
Jackson’s Syndrome
|
X, XI,
XII
|
Intracranial extension
before the nerves leave the skull base
|
|
Tapia Syndrome
|
X, XII, occasionally
|
Lesions high in the
neck
|
|
Cerebellopontine angle
syndrome
|
XI, sympathetic chain ,VII,
VIII, V
|
Extension into CP angle
|
|
Garcin’s hemibase
Syndrome
|
All cranial nerves on one
side (often incomplete)
|
Infiltrative nasopharyngeal
Ca.
|
NEUROIMAGING:
The
cornerstone in the successful management of the jugular foramen lesions is
the preperative high quality and multimodiality neuroimaging.
Advances in this field have led the surgeon to select the most
appropriate surgical approach and technique, to anticipate the possible
complications and to prevent or manage them. CT, MRI and
Angiography of brain must be done in all cases to get the maximum
information preoperatively.
The
plain and contrast CT scan of the brain with 1.5mm cuts, bone window
algorithm and coronal cuts help to reveal the normal bony variation and
the pathological bony involvement, at the site of jugular foramen and
extension into the nearby osseous structures and also the type of
involvement, either expansile (compressive) or invasive (destructive)
enlargement. The presence of obstructive hydrocephalus is also visualized.
If spiral CT scan is available, this, with a bolus of contrast medium
will give additional information like three dimensional
visualization of the skull base and the relationship between the lesions,
vessels and skull base.
MRI
brain images are extremely useful in delineating the exact location,
origin, size, limits, margins, vascularity and extent of the lesions,
degree of involvement of the important neurovascular structures and also
to some extent the pathological diagnosis. For the latter purpose,
a dynamic, high dose Gd-study with creation of time intensity curves is
found to be particularly useful. With this technique glomus
jugulare tumors can be differentiated from schwannoma, meningioma and
metastases. MRI venography is highly predictive in differentiating
pseudomas (large and high lying jugular bulb) from the pathological
lesions. Octerotide scintigraphy, if available, is helpful in the
diagnosis of multifocal paragangliomas since these tumor above 1.5cm size
take up the radiosotope.
|
|
|

|
|
|
Lt.Glomus tumor-MRI axial
|
Lt.Glomus tumor-MRI coronal
|
Lt.Glomus tumor-MRI sagital
|
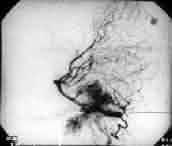
Lt.Glomus tumor-angio
|
Finally
the bilateral cerebral angiography with cross-compression or balloon occlusion
test will demonstrate enlarged feeding arteries, degree of vascularity,
dominance and pathology of sigmoid sinus, jugular bulb and internal
carotid artery. If the tumor is highly vascular, then a
preoperative super-selective endovascular embolization can also be
undertaken to assist in safe surgical removal.
SURGICAL APPROACHES:
Since the
first reported exploration of the jugular bulb for a completely
intraluminal mass by Sieffert in 1934, many surgical approaches, their
modifications and combinations have been developed and utilized by
neurosurgeons and otologists to deal with the jugular foramen
lesions. Historically a sequence in developing these approaches
with the aim to improve surgical management can be distinguished, for
example, realizing the need for VII nerve mobilzation, packing of sigmoid
sinus, ligation of major vessels, resection of the skull base and so
on. As a result, numerous approaches are now available, which vary
in skin incision, soft tissue dissection and bone removal, having
specific indications depending upon the site, size, extend and
vascularity of the tumor, involvement of the surrounding neural (cranial
nerves, brainstem and cerebellum), vascular (internal carotid artery,
vertebral artery, sigmoid sinus, jugular bulb, internal jugular vein and
cavernous sinuses) and osseous (petrous, clivus, condylar part of
occipital bone) structures and finally upon the patient’s clinical
condition (hearing). The choice of the most appropriate surgical
approach to a particular lesion in a particular patient has to be
individualized and is dictated by the morphology of the lesion and the
surgeon’s experience and preference.
The
surgical approaches used for JF lesions, although not always directed
primarily to the jugular foramen, include the suboccipital retrosigmoid,
presigmoid and transsigmoid, retrolabyrinthine and translabyrithine,
transcochlear and subcochlear, trans-supra and juxtacondylar, far lateral
suboccipital, lateral skull base, infratemporal fossa and middle cranial
fossa approaches.
These
approaches can be broadly grouped into posterior, lateral, anterior,
superior and inferior approaches and further subdivided into limited,
extended and combined approaches. In general the limited approaches
are useful for small lesions and extended and combined approaches for the
larger lesions.
Major groups:
|
1. Posterior (through
posterior cranial fossa)
|
Sub occipital retrosigmoid
trans-condylar, supracondylar approaches
|
|
2. Lateral (through
mastoid)
|
Lateral skull base,
juxtacondylar approaches
|
|
3. Anterior
|
Preauricular subtemporal,
infratemporal approaches
|
|
4.
Superior
|
Middle fossa approaches
|
|
5.
Inferior
|
Neck dissection
|
THE
LATERAL APPROACHES:
These
are the most commonly used access routes for the jugular foramen lesions
having large extracranial extensions. These involve basically a
mastoidectomy and more often, anterior re-routing of the VII nerve to
drill the bone inferior to the labyrinth to acess to JF. The
exposure can be widened anteriorly, by sacrificing the external auditory
canal and midline ear structures or medially by drilling away the otic
capsule (translabyrinthine) or cochlea (transcochlear). When
combined with the upper neck dissection it provides a satisfactory
exposure of JF, mastoid air cells, tympanic cavity and extracranial
structures. The removal of styloid process with transposition of
VII nerve facilitates wide opening of extracranial orifice or JF and
provides access to lower part of petrous portion of ICA. Still
wider exposure of extracranial tumour is achieved by removing the transverse
process of atlas or dislocating or resecting the mandibular
condyle. However, these approaches cannot be used for the removal
of large intradural extensions which require combination of the posterior
approaches.
The classification
of Lateral approaches: Juxtacondylar and lateral skull
base approaches.
Lateral
skull base approaches may further be grouped into
-Approaches sacrificing otic capsule (translabyrinthine and
transcochlear)
-Approaches conserving otic Capsule
(extra-labyrinthine)
a) Passing above otic capsule
(supralabyrinthine)
1) middle cranial fossa
2) extended middle cranial fossa
3)
middle fossa
transpetrous
b) Passing behind the otic capsule (retrolabyrinthine)
1) Retrosigmoid
2) Retrolabyrinthine
3) Retrolabyrinthine transtentorial
C) Passing anterior to otic capsule (prelabyrinthine)
1) Infratemporal fossa type B & C (Fisch’) 2)
Preauricular subtemporal – infratemporal
d) Passing inferior to otic capsule (infralabyrinthine)
1) Approaches to jugular foramen
– infra temporal fossa type A & petro-occiptal transsigmoid
(POTS)
2) extreme lateral
approach
THE
POSTERIOR APPROACHES:
These
are the most suitable approaches for the predominantly intradural lesions
and for the Jesions extending down to foramen magnum and medially to
lower and midclivus. The retro-sigmoid approach provides access to
the cere-bellopontine angle and the intracranial orifice of JF. Its
transcondylar modification and the far lateral approach access the
foramen magnum and lower clival regions by opening the posterolateral
quadrant of foramen magnum and by drilling away the posterior part of
occipital condyle. The posterior and posterolateral margin of the
JF is approached by removing the part of jugular process of the occipital
bone behind the JF and the portion of the mastoid just behind the mastoid
segment of VII nerve and the stylomastoid foramen. This provides an
upward view from below but to get a flatter view toward the midclivus, an
additional drilling of jugular tubercle is required.
THE ANTERIOR APPROACHES:
These use the
pathway anterior to the external auditory canal and through the tympanic
bone, exposed by removal or displacement of the glenoid fossa and
temporomandibular joint. The subtemporal-infratemporal fossa
approach alone can access anterior part of JF after reflecting the
petrous portion of ICA anteirorly. Further drilling exposes the
midline and upper clivus anteriorly. However, more commonly this
approach has to be combined with lateral approaches to access the
anterior extension of the pathology. These combined procedures are
designated by Fisch as infratemporal fossa type B and C approaches.
Since
reviewing all the approaches is impossible in this article only the
approaches used in our series are described here.
SUBOCCIPITAL RETROSIGMOID
APPROACH:
This
is a limited and posterior approach pioneered by Sir Charles Balance in
1894 and refined by Cushing and Dandy in 1920, and is frequently, one
component of the more extensive exposures. The main indications are
type A schwannomas of lower cranial nerves, epidermoid cyst and acoustic
neuroma extending down into jugular foramen.
This
is an important standard neurosurgical approach to posterior fossa and
hence does not need elaboration. The retroauricular skin incision
exposes suboccipital region including the asterion and medial portion of
the mastoid process and reaches but does not extend inferiorly to the
supracondylar fossa. Usually the lateral rim of foramen magnum is
life in place. The mastoid air cells are usually opened, taking
care of the emissary veins draining into the sigmoid sinus. The
intracranial part of jugular foramen is exposed by dissecting the
arachnoid around IX, X, XI nerves.
It
is technically simply, familiar and associated with few complications and
can be easily combined with other skull base procedures to gain further
exposure. But, it has limited applicability in that, only
intradural portion of the tumor could be removed and does not allow
removal of either intrajugular pathology or extracranial extensions.
SUBOCCIPITAL TRANSCONDYLAR
APPROACH:
Termed by
Seeger (1978) and refined by Gilsbach (1987) and by Bertalanffy et al,
this approach is an extended modification of the retrosigmoid approach
providing more extended lateral and inferior exposure than the
latter. This is not synonymous to the far lateral approach for the
foramen magnum (FM) lesions, which requires the resection of only the
medial 1/3rd of the occipital condyle. The indications
are intrinsic lesions of the lower brainstem upto pontomedullary
junction, tumors located anterior or anterolaterally to the lower
brainstem, extradural pathology from lower clivus, occipital condyle,
anterolateral rim of foramen magnum and jugular process of occipital bone
and aneurysm of vertebrobasilar complex.
Technique
: Initial procedure is like that of the standard suboccipital
retrosigmoid approach. In addition to suboccipital craniotomy the
bone resection extends to include posterior and medial portion of the
occipital condyle and part of the jugular process superior to the condyle
to expose hypoglossal canal and the jugular foramen from dorsally and
inferiorly. The distal extradural vertebral artery is exposed upto
the point where it pierces the atlanto-occipital membrane and dura.
While making the dural incision it is desirable to leave a cuff around
the vertebral artery, which aids in the watertight dural closure at the
end of the procedure to prevent postoperative CSF leak. The
posterior emissary vein when present is a useful landmark in the
identification of the jugular foramen.
It
provides a straight line view to anterior rim of foramen magnum and lower
clivus, an excellent exposure of lower brainstem without the necessity of
retracting brainstem or overstretching of lower cranial nerves with an
excellent control of vertebral artery in its extradural and intradural
course. It can be extended laterally to expose JF lesions either
from intradural or from extradural approach. The ligation and
division of the sigmoid sinus to expose the intradural portion is done according
to the surgeon’s preference.
There
is a potential risk of injury to vertebral artery (VA), lower cranial
nerves and a risk of craniocervical instability, if the atlanto-occipital
joint is opened. For the predominant extradural growth with a
lateral extension into the JF, Sen and Sekhar used this approach from a
lateral direction by combining lateral exposure of foramen magnum with a
partial mastoidectomy. Though useful for the above indication, the
mastoidectomy and extensive OC resection is not necessary for the
predominant intradural growth.
SUPRACONDYLAR APPROACH:
Described
by Gilsbach et al, this is a limited variation of the transcondylar
approach and is indicated for small lesions confined to hypoglossal canal
and to the medial rim of jugular foramen.
Technique
: Initial procedure is like that of the standard suboccipital
approach. Then the suboccipital craniotomy is extended down to
supracondylar fossa while preserving the foramen magnum and occipital
condyles. The jugular tubercle is drilled away extradurally,
exposing the medial aspect of jugular foramen laterally and hypoglossal
canal inferiorly. The advantage of this approach is the low
morbidity and the disadvantage is that the radical excision is not
possible and is adequate only for biopsy and for small intradural lesions
confined to the hypoglossal canal.
JUXTACONDYLAR APPROACH:
Developed
by Geroge et al, it is an important limited and lateral approach and one
of the primarily targeted approaches to the JF. The prime
indication is the extradural tumors confined to the jugular foramen like
lower cranial nerve schwannoma, meningioma etc.
Technique
: The skin incision starts from superior nuchal line behind the mastoid,
extends along the medial border of the sternomastoid muscle to 6cm below
the mastoid tip. The IJV and XI nerves are exposed after resecting
the muscles attached to the mastoid. The transverse process of
atlas is freed of it muscles attachment and VA above and below the
transverse foramen is exposed. The transverse process of atlas is
removed and VA can be transpositioned, if necessary. The
posterolateral aspects of the atlantooccipital and atlanto-axial joints
are exposed. The posterior belly of diagstric muscle is resected
and occipital artery is ligated. External and internal carotid
arteries are exposed only if necessary. Then a partial
mastoidectomy is done, which is continued medially to expose the distal
SS. The remaining posteroinferior wall of the jugular bulb is
drilled away which opens the jugular foramen posteriorly and
inferiorly. The exposure of VII nerve at its exit at stylomastoid
foramen and at its petrosal segment and the dural opening is done only if
necessary, in cases of large tumors.
provides
a wide exposure of posterolateral aspect of the jugular foramen
with out the extensive petrous bone drilling and hence preserves hearing
and VII nerve functions. There is no risk of CSF leak because dura
is usually not opened. It can be combined with supracondylar
exposure, which is mainly indicated for intradural pathology or with
infratemporal fossa approach Type A.
But
this is a limited exposure of JF with the potential risk of venous
bleeding around the VA within the foramen transversorium of atlas.
Samii
and Bini advocated a combined lateral suboccipital-infralabyrinthine
approach Hirsch, Sekhar and Kamerer proposed a transtemporal and
infratemporal approach for the benign tumors with both extra and
intradural extensions with an excellent control of the vertebral artery.
Post
operative
CSF leak may need repair. Watertight closure with grafts, packing
of the cavity with fat, and use of vascularized muscle flap are used to
prevent CSF leak and its complications. Vascular, and Cranial
nerve injuries may be avoided by choosing the right approach,
meticulous technique with attention to preoperative image studies, and
intraoperative physiological monitoring. Preoperative embolization and
radiotherapy will help.
Hydrocephalus,
craniocervical instability, trismus and incorrect dental occlusion, and
eustachian tube function rarely
occur.
PETRO-OCCIPTAL TRANS-SIGMOID
(POTS) APPROACH
It
is one of the lateral infralabyrinthine skull base approaches primarily
targeting the jugular foramen, described by Mann et al.
It
is primarily indicated for jugular foramen, lesions especially, the lower
cranial nerves schwannoma with intracranial extensions, meningioma of
jugular bulb and some cases of glomus jugulare tumors with predominant
posterior extension. It is also indicated in small petroclival
meningioma lying anterior to internal auditory canal (IAC) with preserved
hearing.
Technique
: A shaped skin incision 4cm posterior to postauricular sulcus with its
lower limb extending inferiorly 2cm below the mastoid up is used.
An inferiorly based ‘U’ shaped musculoperiosteal flap is then raised
extending from 1-2cm above the zygomatic arch superiorly to the level of
mastoid tip inferiorly. Anteriorly a strip of periosteum is left a
few mm posterior to EAC to allow re-suturing of this flap during
closure. The sternomastoid muscle is retracted posteriorly.
The lateral process of atlas is identified and the IJV anterior to this
is dissected free and ligated. Following a complete mastoidectomy
the mastoid portion of VII nerve and JB are identified and the bone over
SS and JB and posterior fossa dura in front of SS are removed. A 4
X 4 cm suboccipital craniotomy is performed limited anteriorly by SS and
superiorly by TS. The infralabyrinthine petrous bone is drilled
away taking care not to injure the posterior semicircular cannal or VII
nerve. The occipital condyle is partially drilled upto hypoglossal
canal. The vertical segment of the JCA is exposed by drilling the
inferior tympanic bone while preserving the EAC wall. The proximal
part of the SS is compressed extraluminally and SS is then opened and
packed distally and proximally. A horizontal dural incision is made
starting posterior to SS, coursing anteriorly transversing the medial
wall of the SS. Then arachnoid is removed from neurovascular
structures, exposing IV-XI nerves and the superior cerebellar artery,
AICA and PICA.
The
removal of lateral wall of JF and if necessary of its medial wall fully
exposes the intracranial part of IX-XI nerves. The dura over the
drilled part of OC is excised exposing the hypoglossal canal. When
needed IX-XI nerves are retracted or sacrificed if invaded by the
tumor. If necessary, drilling is continued to ipsilateral lower
clivus and to lower border of foramen magnum. If control of
vertical portion of ICA and of the infralabyrinthine compartment is
needed, the mastoid segment of VII nerve is mobilized as far as the
stylomastoid foramen. Only if the tumor extends to hypotympanum, an
extended posterior tympanotomy is performed and facial nerve is
rerouted. The retrosigmoid posterior fossa dura should be
closed. The resected cavity is filled with the abdominal fat graft
and the wound is closed.
The
advantages are that the middle ear and VII nerve functions are preserved
and it can be combined with transtentorial approach for tumors with supratentorial
extension or with translabyrinthine approach for tumours involving
IAC in absence of preperative serviceable hearing (and if hearing is
preserved then the posterior and inferior wall of IAC is drilled away
without sacrificing the labyrinth) or with extreme lateral approach for
tumors extending downwards to involve CV junction ventral to the
brainstem.
The
disadvantages are that it only provides limited control of ICA (dorsal
and lateral aspects) and hence extensive involvement of IAC is contraindication
to POTS approach for which either modified transcochlear or infratemporal
fossa type A approach is indicated. Injury to the lower cranial
nerves and CSF leak are the potential complications. Also this is
not useful in highly vascular and invasive glomus jugulare tumour for
which infratemporal fossa type A approach is preferable.
Described
by Ugo Fisch in 1970, it is one of the most important combined approaches
to jugular foramen lesions, belonging to the lateral group of approaches.
Indications
: The jugular foramen lesions especially the large glomus jugulare
tumours, some lower cranial nerves neurinomas and meningiomas and the
lesions of infralabyrinthine and apical portion of petrous temporal bone
like cholestaetoma, chordoma of lower clivus and carcinomas invading this
regions and extensive facial nerve neurinomas.
Technique
: A postauricular skin incision extending superiorly to temporal region
and inferiorly along the anterior border of sternomastoid muscle 5-6 cm
below the mastoid tip with a preaauricular limb is used. A small
anteriorly based musculoperiosteal flap is raised and the cul-de-sac
closure of the external auditory canal is done. Through the neck
dissection, the VII nerve as its exits at stylomastoid foramen is
identified and its main trunk is traced into parotid gland till the
proximal parts of temporal and zygomatic brances. The lower cranial
nerves the ECA, ICA and IJV are exposed in upper neck. After
dividing the sternomastoid muscle and the posterior belly of digastric
muscle, the ECA is ligated distal to its lingual branch. The skin
of external auditory canal, tympanic membrane, malleus and incus are
removed. A radical mastoidecomy is done. The VII nerve is
freed from the fallopian canal from genigulate ganglion to
stylomastoid formamen and transposed anteriorly and fixed to the
new bony canal drilled in the root of zygoma superior to Eustachian tube
and to the tunnel created in parotid gland to lodge the nerve. The
hypotympanum is drilled completely to expose the vertical portion of
ICA. The ascending mandibular ramus is displaced anteriorly and the
mandibular condyle is resected is case of large tumors. The SS is
either packed or doubly ligated and if necessary, its lateral wall is
removed upto the level of jugular bulb and lateral wall of jugular bulb
is opened taking care to pack the IPS and condlar emissary veins entry
into it. The IJV is doubly ligated and cut in the neck and elevated
superiorly taking care not to injure the XI nerve. In case of
limited intradural extension of the tumor, the dura is opened with out
injuring endolymphatic sac.
Advantage
: It offers wide exposure anterior to JF and to infratemporal fossa upto
petrous apex.
Disadvantage
: Apart from hearing loss, facial paralysis and numbness and
malocclusion, this is not suitable for large intracranial tumor extension
and for the large tumors reaching the foramen lacerum or cavernous
sinuses. For this infratemporal fossa Type B or C (anterior
approaches) has to be combined with this type A (lateral approach).
Modifications of this approach
since the
hearing could not be preserved in Type. A Fisch’s infratemporal
fossa approach for the patients with the JF tumor with preserved hearing,
Pensak and Jackler in 1997 advocated an approach that preserves external
auditory canal and middle ear structures and allows working anterior and
posterior to descending segment of VII nerve which is not
re-routed. But this is possible only in tumors that do not erode
the carotid genu.
Sekhar
and Schramm advocated a combined lateral and posterior cranial base
approach (preauricular subtemporal-infratemporal fossa) for large tumors,
which differs from Fisch’s approach in that the VII nerve is not
displaced from the temporal bone.
The
type B infratemporal fossa approach is mainly designed for extradural
petrous apex and midclival tumors, with preservation of the inner ear
function. It is used in associated with type A infratemporal fossa
approach for the extensive glomus tumors involving petrous and the
midclivus. This involves the reflection of zygomatic arch
inferiorly and division of middle meningeal artery and mandibular branch
of V nerve. This gives exposure upto foramen lacerum, petrous apex
and clivus.
The
type C approach involve an orbitozygomatic reflection, sectioning of some
branches of the facial nerve in parotid area, resection of the pterygoid
process and sectioning of V3 nerve. This gives wider exposure to the
carotid artery in cavernous sinus.
One
of the lateral skull base approaches described by Mario Sanna, provides better
visualization of ventral brainstem and vertebrobasilar junction by
removing the petrous apex and clivus and the excellent control of
vertical and horizontal segments of ICA. It is classified into
Types A-D. The Type A is the basic approach upon which other types
are extended, but by itself, it provides only a limited access to tumors
extending into jugular bulb and down to foramen magnum. It is indicated
for extradural lesions involving petrous apex with VII nerve and inner
ear compromise (eg. : petrous bone cholestaetoma, extensive VII nerve
neurinoma, recurrent VIII nerve neurinoma), intradural recurrent VIII
neurinomas, large petroclival meningiomas and for the transdural lesions
invading the petrous bone, like residual glomus tumor, chordoma etc.
Type a modified transcochlear
approach
Technique :
A-C shaped postauricular skin incision is made. The blind sac
closure of external auditory canal, extended mastoidectomy, posterior
re-routing of VII nerve after its complete mobilization from stylomastoid
foramen up to geniculate ganglion and labyrinthectomy are done. The
greater petrosal nerve and vessels are sacrificed. The internal
auditory canal is not opened. The fallopian canal, cochlear and
anterior wall of IAC are drilled and the vertical segment of the internal
carotid artery is exposed. Then pertrous apex and anterior wall of
EAC are drilled. The mandibular condyle is anteriorly
displaced. The petrous apex is drilled upto midelius to get the
full control of horizontal part of ICA. The dura is incised in
front of internal auditory canal taking care not to injure VII nerve.
Its
disadvantages includes risk of injury to VI nerve while incising the dura
of petrous apex and injury to VII nerve while its mobilization.
Type
B modified transcochlear approach incorporate Fisch’s type B or C
infratemporal fossa approach into type A modified transcochlear and is
used for the lesions extending into the parapharyngeal space.
Type C modified transcochlear approach allows control of both
infratentorial and supratentorial parts of tumor lying ventral to pons
and midbrain and is indicated for the petroclival tumors with
supratentorial extension.
Type
D modified transcochlear approach incorporates either POTS or extreme
lateral approach Type A modified transcochlear. This is indicated
in the mid and low clival lesions, petroclival meningiomas and extensive
lower cranial nerve neurinomas. If it is necessary to get excellent
control of the caudal part of the medulla, the VII nerve may be
transposed anteriorly.
POSTOPERATIVE COMPLICATIONS
Many
of the complications are related to the size, vascularity and extent of
the tumor choice of the surgical approach, skill of the surgeon and the
preoperative condition of the patient. Some complications )eg.
Infarct) that are related to preoperative endovascular embolization can
also occur in the post operative period. The possible
complications, their prevention and management are listed in
Table-4. In general, if there are no neurovascular deficits
pre-operatively then meticulous care I to be taken in order to preserve
their functions. In preventing the postoperative CSF leak, which is
the most frequent complication, a lumbar drain is preferred to
intraventricular drain since the latter is fraught with the risk of intraventricular
hemorrhage, which may prove fatal. Excessive CSF drainage is also
to be avoided to prevent the low intracranial pressure and subsequent
subdural hemorrhage. Special mention should be made on the cranial
nerves dysfunction. This is the most serious complication.
The size of the lesion is generally correlated with the dysfunction and
their recovery. In smaller lesions the postoperative morbidity is
minimal and the chance for long term improvement is excellent.
There are reports of excellent long-term recovery in patients in
whom the nerves were sectioned. But more commonly the functional
recovery is dependent on the nerve continuity after the surgery.
Another important point is that if lower cranial nerves dysfunction is
already present preoperatively the patients will be usually compensated
for this deficit and so an aggressive surgical strategy can be undertaken
without producing any increase in their preoperative deficit. In
general the complications can be avoided by carefully scrutinizing, the
preoperative images, selecting the most appropriate approach or its
modification tailored according to the need and by giving enormous
attention to the technical details.
SUMMARY
OF OUR EXPERIENCE
In
our series, the suboccopital retrosigmoid approach was used in two cases
(NO. 1 and 2) of the large acoustic schwannomas extending intradurally
into the jugular foramen and total excision was achieved. For
another large acoustic schwannomas (No.3) extending inferiorly to the
jugular and hypoglossal canal, medially into the petrous bone, clivus,
foramen lacerum and petrous apex and superiorly upto V nerve level, the
modified transcochlear type A approach was used and total excision was
done. In one patient (No. 4) with medium sized dumbbell shaped vagal
schwannoma with a posterior parapharyngeal space-extension, the combined
supracondylar and transcondylar (extended retromastoid) approaches was
used and total excision was done. In case No. 5, the POTS approach
was chosen because the large vagal schwannoma was extending into the
parapharyngeal space, CP angle and eroding the jugular plate, occipital
condyle and near total excision was achieved For the totally
extradural vagal schwannoma (Case No. 6) the juxitacondylar approach was
performed and total excision was achieved. For the small
hypoglossal nerve schwannoma the supracondylar approach was found to be
sufficient for the total removal (No. 9). For the large glomus jugulare
tumors (No. 7 and 8) the infratemporal fossa type A approach was used and
total excision was done, in one case preoperative embolization was used
in another case the preoperative irradiation, to reduce vascularity of
the tumor. The details re given in Table 5.
There
was no mortality in our series and no postoperative CSF leak (we used
fibrin glue and fat graft in selected cases). There were two
instances of new postoperative cranial nerve palsy. Left VII nerve
in case No. 7 and left X nerve in case No. 1. The temporary
deterioration of preoperative nerves dysfunction (VII, VIII, X, XI) was
seen in almost all cases and most of them improved after two to three
months. There are no other significant complications occurred in
our cases. In all cases the postoperative CT and / or MRI
were done for the follow up study and there was not recurrence or
residual tumor seen.
DETAILS
OF AUTHORS’ CASES
|
No
|
Age/Sex
|
Hospital stay
|
Symptoms
|
Signs
|
Duration
|
Diagnosis
|
|
1
|
28y/F
|
21 days
|
Seizures,
headache, deafness Lt ear& facial weakness &
numbness
|
Lt V1,2,3Lt.VII,VIII N
palsy, Lt. Cerebellar signs
|
1yr
|
Lt 8th nerve schwanoma
|
|
2
|
60y/M
|
30 days
|
Rt.
Sided weakness,tremor, imbalance while walking, facial
weakness.
Operated elsewhere In December ‘99
|
Rt 7,8,9,10th nerve palsy
with cerebellar signs.
|
1yr
|
Lt.8thnerve
residual schwanoma.
|
|
3
|
56y/F
|
15 days
|
Tinnitus
Lt ear, pain in the neck, vertigo, facial
weakness
|
Lt.5,7,8,10,11nerve palsy
with cerebellar signs
|
6mths
|
Lt.8th nerve schwanoma
|
|
4
|
58y/M
|
31 days
|
Right
ear pain, right neck swelling,
dyshagia, dysphonia
|
Rt. 9th and 10th palsy and a
lump in the neck
|
10yrs
|
Rt.10th nerve schwanoma
|
|
5
|
32y/M
|
27 days
|
Unsteady
gait, vertigo, Tinnitus, decreased hearing(Lt ear) dysarthia, Lt
shoulder and arm weakness
|
Lt LMN 7,8,9 and 11
palsy
|
1yr
|
Rt.10th nerve schwanoma
|
|
6
|
41y/F
|
25 days
|
Rt.neck pain, occasional
regurgitation, operated elsewhere in 97 for Rt neck swelling,
dysphagia, hoarseness
|
Rt X, XII, N palsy
|
1yr
|
Rt.10th nerve schwanoma
|
|
7
|
17y/M
|
30 days
|
Tinnitus,
deafness(left ear), dysphagia, dysarthria
|
Lt VIII, X & XI
palsy
|
1yr
|
Lt.glomus jugulare
|
|
8
|
42y/F
|
18 days
|
Discharge
from Lt ear (operated in 1984) elsewhere for hoarseness,
dysphagia
|
Lt VIII nerve palsy
|
8mths
|
Lt.glomus jugulare
paraganglioma
|
|
9
|
50y/F
|
17 days
|
Wasting
and weakness of tongue Lt side, swelling in Lt side of neck,
hoarseness, dysarthria, Lt shoulder weakness
|
Lt X, XI, XII palsy
|
3 yrs
|
Rt.12th nerve schwanoma
|
CONCLUSION
It
is true that the outcome in patients with jugular foramen lesions has
dramatically improved during the last two decades, owing to the
sophisticated technical advances in imaging techniques and micro neurosurgical
tools which, in turn, made the surgeon to get maximum information
regarding the detailed morphology of the lesions and to achieve the
principle of minimal invasive surgery, respectively. Equally
important is the surgeons’ ability in selecting the patient and tailoring
the surgical approach based on the morphological and biological criteria
of the lesions and on the preoperative clinical status of the patient,
and more importantly in applying the good old principle of ‘to do no more
harm’ to the patient and finally in showing an intense quest for gaining
more knowledge and acquiring never surgical skills to aid in the
patient’s management. In spite of these achievements we still see
some patients suffering from the disabling morbidity either due to the
disease per se or to the postoperative sequealae. Interestingly and
also unfortunately, we have yet to get the benefit from the basic
neurosciences research work (neurobiology,molecular genetics, cloning,
neurochemistry etc.,) because of its slow pace of progression for the
obvious ethical issues and technological inadequacy. If it becomes
available then we can think of successful neural grafting or
microelectrode implantation for cochlea, pharyngeal and laryngeal muscle
‘pacing’ etc and ultimately of a 100% success rate in the management of
the jugular foramen lesions.
That
day will come soon ! we hope!!
|