|
Skull fractures, that are fractures of the cranial vault and
base of skull, excluding facial fractures, are the results of significant
force to the head and are classified according to the integrity of the
overlying skin, the site, the shape of the fracture and the final
position of the bony fragments. As a result of the force applied
there is often associated brain injury.
Skull fractures in all but the neonate are caused by
significant impact force to the cranium and may be associated with a
variety of other injuries, both intracranial and extracranial. The
cranial vault develops form membranous bone, with ossification of the
bones commencing at six weeks gestation and the syndesmotic sutures
fusing by the fifth decade. Growth of the skull vault is driven by
the growth of the underlying brain, with maximum rate of growth in the
first twelve months during which time the brain doubles its weight.
Growth of the skull is complete by ten to twelve years. This development
of the skull is important as different types of fractures occur in the
different age groups.
Incidence:
Simple linear fractures constitutes about 50% of all, and
the compound fractures about 25%. Simple depressed fractures make up
about 6 %.
Mechanisms of injury:
The biomechanics of skull fractures depend on a direct force
being applied to the skull, surface area of the force,
velocity of the force, point impact, and the age of the patient.
If the force is applied over a longer time it will result in
acceleration of the head. Bone in the adult and older child, has great
resistance to compression but little resistance to tensile strain, and
thus when direct force is applied to the skull, the skull is deformed
instantaneously with the weaker tensile strength resulting in the inner
table fracturing initially and if the force is of sufficient
strength then the outer table will also fracture. These findings
are not true for young children where the bone still has elastic
properties and can therefore be deformed without fracturing. The
propagation of the fracture depends on the force applied and the local
anatomy, namely, the thickness of the bone and the presence of bony
ridges.
Sutural diastasis can occur in young patients without
significant force, but in the adult patient with fused sutures it is a
sign of significant trauma and may well be associated with intracranial
complications.
Remote effects of
forces applied to the skull can result in fractures at a site distant to that
of the impact, due to the transmission of energy through the facial bones
or with the development of a release fracture. With the application of a
force to the skull, the shortening of a skull diameter in line with the
force of lengthening of the diameter at right angles to the force causes
a reversal of the energy forms, with the compressive strain on the inner
table and the tensile strain on the outer table.
Diagnosis:
Simple linear fractures may only present with a boggy scalp
swelling, with a range of neurological signs and varying levels of
consciousness. Compound fractures may well have associated evidence of a
dural laceration with CSF leak or brain herniating through the
wound.
Radiology:
|
Skull X-rays have been the standard radiological investigation
in head injuries, and still have their place, even with the
introduction of CT scans. The advantages of skull x-rays are, the
majority of linear fractures are revealed, air fluid levels are well
shown within the para-nasal sinuses and cranium, the cranio-cervical
junction is well delineated on skull x-rays, the majority of adult
patients have a calcified pineal gland and therefore in departments
with no access to CT scans, a skull x-ray may reveal midline shift due
to a mass lesion, management plans can be made on the result of a skull
x-ray. The diagnosis
of a base of skull fracture remains clinical and may not be shown on
skull x-rays but the associated radiological signs of pneumocephaly and
air-fluid level in the frontal or sphenoid sinuses suggest the presence
of such a fracture.
|
|

|
|
Linear fracture-plain X-ray
|
|
Patients who require a CT scan do not
require a skull x-ray.
CT Scanning has revolutionized the management of
trauma, in particularly head injuries, with good resolution of the
cranial vault on axial bone windows’ and the intracranial contents on
‘soft tissue windows’, but there are limitations with imaging the
posterior fossa and for base of skull imaging coronal scans must be
done. Two dimensional CT scanning in trauma patients is sufficient
in the radiological assessment of skull fractures, with no further
information gained from three dimensional scanning.
Magnetic resonance imaging
is not superior to CT scanning in the acute assessment of head injured
patients, due to the length of time taken for each scan, the use of non
ferro-magnetic anesthetic equipment and the poor resolution of the bone.
CLASSIFICATION:
Fractures of the cranial vault and base of skull are the
results of significant force to the head and are classified according to
the integrity of the overlying skin, the site, the shape of the fracture
and the final position of the bony fragments. As a result of the
force applied there is often associated brain injury. The
classification is important as it highlights the various complications,
as well as the different approaches to their management.
There are many systems to classify skull fractures, as
listed below; however the most practical system is a combination of all
three:
· Linear, or
displaced (slot, comminuted, depressed or elevated) skull fractures.
· Simple or
compound (related externally to the integrity of the overlying scalp
and/or internally involving the paranasal air sinuses, or mastoid air
cells)
·
Anatomically, base of skull or vault fractures.
|
Linear fractures:
These fractures are significant if the
fracture line crosses a meningeal artery or one of its branches (may
lead to extradural hemorrhage), a dural venous sinus (may result in
venous thrombosis, headache, and seizures), and extends into the
paranasal sinuses. In the base it usually skirts the foramina because
of the strong buttresses of bone around the foramina.
Compound fractures carries the risk of
infection and cortical thrombophlebitis and require thorough
debridement and prophylactic antibiotics.
In children, these fractures are often
widely separated (usually lambdoid sutural diastasis) and usually heal
by union within few months unlike in adults.
|
|
|
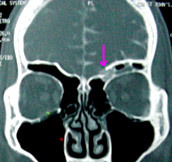
Growing fracture (Cranio-cerebral erosion):
|
Linear fracture-CT scan
|
In children, some linear fractures are associated with torn
dura due to dense attachment of the dura to the bone in this age group. A
rare complication, which occurs in 0.6% of linear skull fractures in
pediatric patients: 90% occur before the age of three. The fracture is
associated with a dural tear, preventing primary dural healing and
resulting in progressive enlargement and eversion of the fracture line.
The arachnoid sac may contain CSF and herniated brain with or without porencephaly.
The treatment for the two forms is different, as the former requires a
duro-cranioplasty (debridement of the damaged brain and dural
repair) whilst the latter a shunt, in order to prevent progressive
neurological deterioration.
Displaced fracture:
Simple depressed
fracture are more common in children. Birth injuries, and fall from a
height are the common causes. Any depression more than 5 mm is likely to
have injured the dura. In a pond fracture, the inner table and the
dura are intact.
Surgical elevation is recommended by many. Others argue that
the damage occurs at the time of injury and elevation do not help. No
reliable data is available to support surgery except for cosmetic
purposes. Elevation over a sinus area may be hazardous.
|
|

|
|
|
|
Depressed
fracture-CT
|
Depressed fracture-3D
CT
|
Pond fracture
|
Elevated
fracture
|
Compound depressed
fracture is an emergency to prevent infective sequelae.
Surgery for these patients is initial local wound closure
after thorough cleaning and removal of foreign bodies, to achieve
hemostasis and prevent infection. If there is no dural laceration this
will be the definitive treatment.
Definitive surgery must be performed as soon as possible, if
there is a suspected dural laceration or intracranial hematoma or
moderate to severe wound contamination. Dural laceration should be suspected
if there is CSF in the wound, brain herniation, pneumocephaly in the
absence of a base of skull fracture or on imaging there is intracranial
air, the outer table of the skull is depressed below the inner table(or
any depression above 5 mm), or a spicule of bone within the cranium
The surgical principles are:
·
Thorough cleaning of the wound with great attention to removal of all
foreign bodies and debridement of devitalized scalp.
·
Removal of the bone around the fracture with a craniotomy or craniectomy
to reveal a margin of normal dura and then removing the depressed
fragment without causing further cortical laceration.
·
Define the dural edges and extend the opening to inspect the underlying
brain, evacuate intradural hematoma, foreign bodies and achieve
hemostasis.
·
Dural closure, with primary suturing if there is no significant dural
loss; however if there is a large dural defect, a duraplasty must be
performed, using pericranium, fascia lata or an appropriate xenograft.
·
Bone fragments can be replaced if the wound is thoroughly cleaned, there
is no clinical evidence of wound infection, the surgery is
performed within 24 hours of injury and the patient is treated with the
appropriate antibiotics .
·
Frontal depressed fractures with associated facial fractures should be
treated acutely as a combined procedure, as patients who have a high
Glasgow Coma Score, no evidence of raised ICP or displacement of midline
structures, do not appear to have an increase in operative morbidity .
Earlier approaches to the management were with two or three operations,
the initial neurosurgical procedure followed 7 to 10 days later by
maxillo-facial reconstruction; however acute surgery is possible with
improvements in neuroanesthesia, neurointensive care and the new plating
sets for reducing and fixing these fractures.
·
Scalp wound must be closed primarily or if there is a large skin defect
the scalp can be ‘expanded’ by making parallel release incisions in the
galea parallel to the wound or using a rotation flap to cover the
fracture, with skin grafting the donor site.
Compound
elevated fractures are caused by tangential injuries which slice off
a portion of the scalp, skull and the underlying dura.
Slot fractures are always contaminated and
are due to penetrating trauma caused by a blade, axe or machete, and
therefore usually associated with a dural laceration. Principles of
treatment are the same as in compound depressed fractures.
|
Basal fractures:
The local anatomy of the skull base, with the paranasal
sinuses and mastoid air cells in
close proximity to the dura, usually renders these
fractures compound.
There has been no adequate controlled study to assess the
benefit of prophylactic antibiotics
in the prevention of post-traumatic meningitis in patients
with base of skull fractures. The
working party of the British Society for Antimicrobial
Chemotherapy recommends close
monitoring of patients to diagnose meningitis early and
treat appropriately.
Base of skull fractures can be sub-divided anatomically
into the fossae namely, anterior,
middle and posterior fossa fractures.
Anterior Fossa Fractures may be presumed
with scalp emphysema,peri-
orbital hematomas/panda or raccoon eyes where there is
subconjuntival hemorrhage with
no posterior limit, epistaxis, anosmia, CSF
rhinorrhoea, or blindness, suggest an anterior
fossa fracture.
Epistaxis is usually managed with adequate nasal packing.
The olfactory nerve filaments are fine and delicate and
can get injured in cribriform
plate fractures. Anosmia may be missed in acute stages. An
associated dural tear may result
in CSF rhinorrhoea; it usually stops in 3-4 days.
Persistent cases require a repair.
Optic foramen
region fractures may result in optic nerve injuries and warrant immediate
attention.
Pneumocephalus, due
to entry of air from the sinuses, is an emergency. The patient develops
a tension pneumocephalus due to a dural flap valve or with the use of
positive airway pressure
with an anaesthetic
mask. A twist drill to let out the air may be life saving.
Middle fossa
fractures often extend to anterior fossa and posteriorly to petrous
pyramid.
Blood in the
external auditory meatus, deafness, facial palsy, or delayed appearance
of subgaleal altered blood over the mastoid ( Battle sign) may point to
a middle fossa fracture.
The fracture may
also injure the cavernous sinus, and may result in carotico-cavernous
fistula.
|
|
|
|
Contrast cisternography-CSF
leak thru' ant cranial fossa fracture
|
|

|
|
Fracture cribriform plate with CSF rhinorrhoea
|
|

|
|
Traumatic
penumocephalus
|
|
|
|
The 3rd, the 4th, and the 6th nerves are at risk. The 3rd
nerve paresis in patients with a normal level of consciousness are due to
traction injuries, however if a sign of transtentorial herniation, the
third nerve palsy will be preceded by a decrease in the patient’s level
of consciousness. The 4th nerve has the long subarachnoid course and may
sustain traction injury. The 5th nerve lies in the lateral wall of the
cavernous sinus with the three divisions exiting through the middle
fossa, where fractures can injury the nerve directly. The 6th nerve
is tethered by the posterior cerebral and superior cerebellar arteries as
it exits the brain stem and as it enters the cavernous sinus through
Dorello’s canal, therefore any shift in the brain stem relative to the
base of skull can cause traction on this nerve.
Longitudinal fracture due to a lateral blow is common, and
may result in facial nerve injury. The less common transverse
fracture as a result of occipital blows involve the 7th and 8th nerves
along with disruption of vestibular and cochlear components of the
labyrinth. The facial nerve is susceptible to injury within the petrous
bone from middle fossa fractures. Facial nerve palsy immediately
after the injury suggests traction, torsion or tearing of the nerve,
whilst those that are of delayed onset are due to nerve swelling or a
compressive haematoma in the facial canal and both groups of patients may
be treated conservatively as the recovery of facial nerve function is
91.7% in the former and 94.1% in the later. Some surgeons recommend
large doses of steroids to prevent a delayed facial palsy. Surgical decompression/
repair via transmastoid translabyrinthine approach is being tried
in facial nerve injuries with varying reports.
Deafness from a middle fossa fracture, if
associated with a facial palsy, suggests a neural injury. If not,
ossicular dislocation must be excluded as this is a treatable form of
deafness. Therefore all patients with a middle fossa base of skull
fracture must have full hearing assessment within two weeks of injury.
|
CSF otorrhoea is rare and subsides
spontaneously almost invariably.
CSF rhinorrhoea (with an intact
tympanic membrane) may require surgical intervention.
Pituitary failure
is rare complication, but should be suspected if the patient has
bilaterally dilated pupils and refractory hypertension. The
majority of these patients has a disrupted optic chiasm as well as
disrupted pituitary stalk
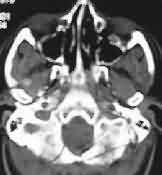
Post. fossa
fractures are rare. associated cervical spine injuries must be ruled
out.. The 6th to12th nerves may be injured.
|
|
|
|
Posterior fossa fracture-CT scan
|
CONCLUSION:
Skull fractures, per se may be of no clinical significance,
however when associated with decreased level of consciousness, or a focal
neurological deficit, it may be an indicator of an intracranial hematoma
or cortical contusion. A force severe enough to fracture the skull may
produce brain damage as well.
The risk of intracranial hematomas in adults and pediatric
patients with head injuries depends on two important clinical findings,
namely, a skull fracture and the patient’s level of consciousness. The
risks of intracranial hemorrhage (extradural, subdural, intracerebral)
following a skull fracture depend on the age and the level of
consciousness of the patient. 1 in 12 of children and 1 in 4
of adults with decreased GCS and fracture, have an ICH.
Infection results from delayed treatment or inadequate
treatment of the compound fractures, ranging from superficial wound
infection to the more severe intracranial complications of meningitis,
subdural empyema or brain abscess.
Hence a skull fracture should alert the neurosurgeon when
patients, with a history of head injury, present with a neurological
problem.
|