|
In
1817, Parkinson, in the classic �Essay on the Shaking Palsy�,
described a novel condition that now bears his name. He described
the cardinal manifestations: tremor, bradykinesia, gait and postural
disturbance. Charcot, who was so impressed by Parkinson�s
description that he called the constellation of symptoms
Parkinson�s disease, expanded description of the disease in the
nineteenth century - named paralysis agitans by Marshall Hall
in 1841.
Parkinson�s
disease accounts for 75% of cases of Parkinsonism .
The
current surgical population is distinct from those treated before
the use of L-dopa. Today�s surgical candidate is more likely to
have true idiopathic PD and likely has been treated with several
medications before surgery. For many, surgery is performed to
eliminate l-dopa-induced dyskinesia, an iatrogenic condition that
did not exist before the introduction of L-dopa therapy, and one
that may be unavoidable no matter how L-dopa is administered.
Physiologic
basis of surgery:
The
development of primate models of PD and the refinement of single
cell microelectrode recording have resulted in a vastly improved
understanding of PD pathophysiology. The following three points are
essential to understand current surgical approaches:
1.
Although
an intact pallidothalamocortical loop is necessary to exhibit
tremor, lab data suggest that tremor activity is probably generated
in the ventrolateral nucleus of the thalamus. These data support the
clinical observation that lesions or high-frequency stimulation in
this region best treat parkinsonian and essential tremor.
2.
The
striatum modulates activity in the globus pallidus pars interna(GPi)
both directly and indirectly, via the globus pallidus pars
externa(GPe) and the subthalamic nucleus(STN). In PD, loss of
dopaminergic input to the striatum leads to a reduction in direct
pathway activity and an increase in activity along the indirect
pathway, changes that result in STN and GPi hyperactivity. The
output from GPi to
ventrolateral thalamus is inhibitory, reducing the excitatory
thalamic input to supplementary motor areas that are critical to the
normal execution of movement. Thus hyperinhibitory outflow from GPi
may account for the negative symptoms of PD(i.e., rigidity and
bradykinesia). Reduction of this excessive inhibitory outflow, by
lesioning or chronically stimulating GPi or STN, can reverse these
symptoms.
3.
With
time, differential sensitivities of the direct and indirect pathways
to L-dopa therapy may occur. This imbalanced response to exogenous
L-dopa may result in choreiform movements that characterize L-dopa
induced dyskinesias. It is not completely clear, however, why
ablating GPi eliminates this condition.
The
advent of axial computed tomography and then magnetic resonance
imaging has altered stereotactic technique. Employing these imaging
modalities with modern stereotactic frames, the position of deep
brain targets can now be sited directly, not estimated on
ventriculograms. Nevertheless, current MR imaging does not always
demonstrate deep brain structures (such as specific thalamic
subnuclei) with sufficient resolution for it to be the sole means of
targeting. Moreover, MR imaging is prone to distortions. Although
typically small, they can be large enough to affect targeting for
these types of procedures. Therefore some type of intraoperative
physiologic confirmation is essential for performing successful
movement disorder surgery.
Microelectrode,
semimicroelectrode and macroelectrode techniques have been
described. Microelectrode recording yields the highest quality
localizing information, so that lesioning or DBS implantation can be
performed with greatest confidence. Concerns that the increased
number of trajectories employed with microelectrode recording
increases the risk of hemorrhage have not been substantiated;
however it is questionable whether the extra time, effort and
expense of performing these are necessary to achieve results.
Neuroablative
procedures:
The
goal of neuroablation is to disrupt irreversibly an abnormally
functioning structure (usually a nucleus), leaving volitional
movement intact. Ideally the lesion is just large enough to achieve
the desired result but not so large as to cause collateral damage.
During the first half of the twentieth century, neurosurgeons
lesioned numerous sites throughout the motor system, searching for
the ideal target. Lesions within the ventrolateral thalamus and GPi
have yielded the best results. Many lesioning techniques have been
employed � radiofrequency thermocoagulation is the most commonly
used modality because of its reliability and simplicity.
Ventrolateral
thalamotomy:
Hassler and Reichert are credited with making the initial foray into
the ventrolateral thalamus, reporting improvement in both tremor and
rigidity. Thalamotomy thereafter became the favored surgery in the
pre-dopa era because the surgical response is instantaneous and more
easily monitored than the response to pallidotomy. A number of
surgeons have reported excellent long-term and short-term tremor
suppression after thalamotomy, although contemporary authors do not
report significant improvements in rigidity or bradykinesia. Tremor
may be suppressed with lesions anywhere within the ventrolateral
thalamus, but the ventralis intermedius subnucleus of the
ventrolateral thalamus is considered by most to be the ideal target.
The surgical mortality rate for thalamotomy is less than 0.5%;
typically resulting from intracerebral hemorrhage. Morbidity may
vary from 9-23% - but has decreased due to improved lesioning
technique, and patient selection. Dysarthria and contralateral
hemiparesis are the most common adverse events. Speech difficulties
are even more prevalent in those undergoing bilateral procedures.
Dystonia, hemiballism and athetosis have also been reported. In most
instances, PD causes a resting tremor that diminishes with action,
making this symptom one of the least disabling, and its elimination
does not improve the functioning of the patient. Therefore it has
given way to pallidotomy which addresses disabling PD symptoms such
as rigidity, dystonia and dyskinesia.
Pallidotomy:
in 1960 Svennilson et al reported superior results with pallidotomy
by placing the lesion posterior, inferior and lateral to the
previously described pallidotomy site. This was exemplified in the
work done by Laitinen et al in 1992. Posteroventral pallidotomy
dramatically improved rigidity, bradykinesia, tremor and ambulation
in the majority of moderately advanced PD patients. Most important
was the discovery that pallidotomy reduced or eliminated dyskinesias
induced by dopa. It has been proved that pallidotomy reduces or
eliminates dopa-induced dyskinesias, rigidity, muscular spasms and
off state dystonia in patients with idiopathic PD who are still dopa
responsive, but suffer from motor fluctuations. Tremor may also
improve, but not as consistently as with thalamotomy. It improves
the off state function and prolonged on states that are free of
dyskinesia. Up to 60% improvements with effects lasting for 2 years
have been reported.
The
most frequent complication is visual field deficit (14%) � due to
extension of the lesion into the optic tract. Injury to the internal
capsule, facial paresis and cognitive deficits may occur.
Complications increase with bilateral procedures � speech,
swallowing and cognition.
Gamma
pallidotomy and thalamotomy:
Leksell originally conceived the gamma knife to perform stereotactic
neuroablative procedures without open surgery. But its use was
limited by inadequate imaging. With high resolution MRI gamma knife
surgery for neuroablation has become a reality. Only a few cases of
thalamotomy and pallidotomy have been reported; the rate of
improvement is lower than that for conventional procedures (50%).
Disadvantage being that the patient has to wait for weeks to months
to notice any positive changes. Therefore clinical
efficacy/potential complications cannot be determined at time of
surgery.
|
Deep
brain stimulation:
The
idea for long-term DBS arose from the observation that
high-frequency stimulation of the ventrolateral thalamus
arrests tremor, a phenomenon that is employed for
physiologic localization of the thalamotomy target. If one
can arrest tremor with stimulation, why lesion? The
advantages of DBS are � a reversible, functional lesion is
made in lieu of a permanent anatomic one, stimulation
parameters can be adjusted over time to maintain tremor
suppression in the event of disease progression. The
disadvantage being cost and maintenance of the device. The
deep brain electrode is placed through a burr hole. As with
the lesioning procedures the patient is awake and his
neurologic status can be assessed throughout. Once placed
correctly, the electrode is anchored to the skull. As the
electrode is flexible, it can move with the brain and
maintain its anatomic location. Each electrode has four
contacts. Stimulation can be performed in monopolar bipolar
fashion. Once acceptable stimulation parameters have been
identified for the patient, they are programmed into the
implantable pulse generator, which, similar to a cardiac
pacemaker is placed within a subcutaneous pocket below the
clavicle and connected to the electrode via wires that are
tunneled beneath the skin. Stimulation parameters may be
adjusted at any time employing a transcutaneous programmer.
A magnet may be used to turn the stimulator off at night or
to switch between two stimulator settings.
The
mechanism through which DBS achieves its functional results
is presently unclear. Stimulation may create a
depolarization block, jamming the signals emanating from an
abnormally functioning structure, although this is
unsupported by more recent findings. Alternatively
antedromic and orthodromic propagation of the depolarization
may affect distant structures that transmit to or receive
impulses from the stimulation target.
Thalamic
deep brain stimulation:
Initially
Benabid et al employed thalamic stimulators contra lateral
to previously successful thalamotomies in patients with
bilateral tremor to reduce the risk associated with
bilateral thalamotomy. The results demonstrated that
thalamic DBS achieves tremor suppression with an equivalent
efficacy to thalamotomy.
The
tremor suppression was dramatic and significant. Tasker
retrospectively compared DBS and thalamotomy performed in
one venter, and found that initial tremor suppression was
comparable in both, but tremor recurrence was higher (15%
versus 5%) in the thalamotomy group. Tremor recurrence
necessitated reoperation in the thalamotomy group, while it
could be resuppressed with adjustments to the stimulation
parameters in the DBS group.
Neurologic
complications were less frequent in DBS group and could be
controlled with stimulator adjustments. Painful dysesthesias
secondary to stimulation of the ventrocaudal nucleus (lies
immediately posterior to the ventralis intermedius);
dysarthria; and dystonia are the predominant complications.
Hemorrhage rates and congnitive difficulties may be less
frequent.
|
 |
|
Radio
frequency lesion generator and electrode.
|
 |
|
Ideal
target location for Posteroventral Pallidotomy
|
|
|
Ideal
target location for Subthalamic nucleus.
|
|
|
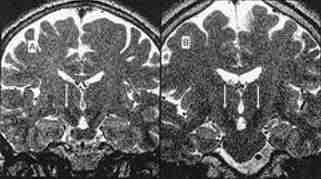
subthalamic nucleus as seen on T2W
|
|
Pallidal
stimulation:
In
1994 Siegfried and Lippitz reported their initial experience
performing bilateral pallidal DBS implants. Significant motor
improvements comparable to pallidotomy were achieved. Rigidity and
dyskinesias were the most responsive symptoms. Gait difficulties are
helped less. Ventral stimulation eliminates dyskinesias and rigidity
but worsens akinesia whereas dorsal GPi stimulation reduces akinesia
but may worsen dyskinesia. This made pallidal stimulation to have a
narrow therapeutic window.
Subthalamic
nucleus stimulation:
Limousin
et al and Pollak et al demonstrated that bilateral STN stimulation
is safe and improves akinesia and gait abnormalities. These two are
the most disabling and medically resistant sequelae of PD, they do
not improve after lesioning or stimulation in the thalamus or
GPi. STN ablation is not done because lesions there cause a
medically resistant, violent hemiballism. Additional benefit of STN
DBS is the reduction in requirement of l-dopa after surgery. Krack
et al reported improvements in tremor and off state dystonia in
large series on patients. Dyskinesia is reduced secondarily by
medication reductions.
Preoperative
evaluation:
Patients
should not be considered surgical candidates until all reasonable
medication strategies have been tested. Initially a movement
disorders neurologist, who confirms the diagnosis of PD and makes
sure that the patient is truly medically refractory, evaluates the
patient. The surgeon then evaluated by a neurosurgeon who decides
which surgery would best addresses the patient�s symptoms.
Patients must have a recent MRI to rule out concurrent neurologic
disease � multiple infarctions, cerebral atrophy. Detailed
neurosphsychological testing is performed to rule out co-morbid
dementia, a common sequela of PD that can be worsened by surgery. If
an elderly patient stands to gain significant functional benefit
from alleviation of surgically treatable symptoms and meets all the
selection criteria, surgery is offered. But is the patient has
advanced PD, is bedridden, l-dopa unresponsive and contracted, no
surgery is offered.
Selecting
the proper procedure:
1.
Those
who still respond to L-dopa therapy but less consistently are
asymmetric in their symptoms, and plagued by motor fluctuations and
dopa-induced dyskinesia are excellent candidates for pallidotomy/stimulation.
Patients with off state dystonia or muscle cramping will also
benefit.
2.
In
patients with bilateral dyskinesia, staged bilateral pallidotomy/bilateral
stimulators may be considered.
3.
In
the rare PD patient who is truly tremor predominant thalamotomy or
thalamic stimulation is the choice.
For
those with significant gait disturbances, a predominance of axial
symptoms and medically resistant akinesia, bilateral STN or GPi
stimulators is the only viable options.
|
Procedure
|
Tremor
|
Dyskinesia
|
Rigidity
|
Bradykinesia
|
Off
state dystonia
|
Freezing
|
Gait
disturbance
|
|
Thalamotoy
/thalamic stimulation
|
+++
|
+
|
+
|
-
|
+
|
-
|
-
|
|
Pallidotomy
|
++
|
+++
|
+++
|
++
|
+++
|
+
|
+
|
|
Pallidal
DBS
|
++
|
+++
|
+++
|
++
|
+++
|
++
|
++
|
|
STN
DBS
|
++
|
++
|
+++
|
++
|
++
|
+++
|
++
|
Refinements
in the understanding of the anatomic, physiologic and the
neurochemical underpinnings of Parkinson's disease have greatly
contributed to this renewed interest in neuroablative surgery and
are giving rise to newer, more sophisticated therapies. Modern
stereotactic technique permits targeting with millimeter accuracy.
Deep brain stimulation has been introduced as an alternative to
neuroablation. It is hoped that cellular transplantation or virally
mediated gene transfer therapies that seek to restore or preserve
function will soon be clinically viable.
|