|
“ Watson, come here I want you” said Alexander Graham Bell
on March 20, 1876, when he inadvertently spilled battery acid on himself,
while making the world’s first telephone call. Little did Bell realize
that this was indeed the world’s first telemedical consultation. We have
come a long way since then. Today even tele surgery is a reality. This
article will briefly review some aspects of Telemedicine particularly its
relevance in a developing country like India and the experience of the
Apollo Hospitals in setting up telemedicine centers.
Introduction:
Secondary and tertiary medical expertise is not available in
several areas of the world. Quite often, many patients are sent elsewhere
at considerable expense. In a number of these cases the treatment could
have been carried out by the local doctor with advice from a specialist.
Even within a country there is a tendency for specialists to concentrate
in the big cities making medical care in suburban and rural areas sub
optimal Using a PC, a scanner, a digital camera networking, appropriate
software and telecommunications it will be possible to transfer clinical
data from any part of the world to any other part.
Offering medical advice remotely, using state of the art
telecommunication tools is now a regular feature in several parts of the
world. Several studies have shown telemedicine to be practical,
safe and cost effective.. Telemedicine hinges on transfer of text,
reports, voice, images and video, between geographically separated
locations Success relates to the efficiency and effectiveness of the
transfer of information
What is
Telemedicine?
Telemedicine is a method, by which
patients can be examined, investigated, monitored and treated, with the
patient and the doctor located in different places. Tele is a Greek word
meaning “distance “and Mederi is a Latin word meaning, “to heal”. Time
magazine called Telemedicine “healing by wire”. Though initially
considered “futuristic” and “experimental” Telemedicine is today a
reality and has come to stay. In Telemedicine one transfers the
expertise, not the patient. Hospitals of the future will drain patients
from all over the world without geographical limitations. In Cyberia
after all one is a netizen! High quality medical services can be brought
to the patient, rather than transporting the patient to distant and
expensive tertiary care centres. A major goal of telemedicine is to
eliminate unnecessary travelling of patients and their escorts. Image
acquisition, image storage, image display and processing, and image
transfer represent the basis of telemedicine. Telemedicine is becoming an
integral part of health care services in several countries including the
UK, USA, Canada, Italy, Germany, Japan, Greece, and Norway and now in
India.
What is the relevance of
telemedicine in a developing country like India and particularly in the
specialities?
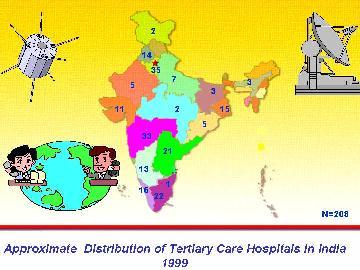
The following table indicates the ground realities of the
present state of health care in India.
|
Health Scenario in
India:
620 million live in rural India
(NCAER)
Bed-Population ratio 1:1333 (1991) Vs.
ideal of 1:500
2 million beds are required as
against0.7 million available.
700 hospitals of 250 beds each are
required every year.
only 9% of 1 billion people are
covered health schemes.
only 0.9% of GDP for health (WHO
recommends 5%)
5% of annual family income spent
towards curative health care.
¯ Specialists relocating to sub-urban or
rural areas
|
|
In Utopia, every citizen has immediate access to the
appropriate specialist for medical consultation. In the real world this
cannot even be a dream. It is a fact of life that “ All Men are equal,
but some are more equal than others ”. We are at present, unable to
provide even total primary medical care in the rural areas. Secondary and
tertiary medical care is not uniformly available even in suburban and
urban areas. Incentives to entice specialists to practice in suburban
areas have failed. After all professional isolation would lead to
mediocrity, which is one step away from entering the Jurassic Park.
‘Health for All’ may be a slogan even in 2020.
It is generally considered that communities most likely to
benefit from telemedicine are those least likely to afford it or have the
requisite communication infrastructure.
This may no longer be true. In contrast to the bleak
scenario in health care, computer literacy is fast developing. Prices are
falling. Health care providers are now looking at Telemedicine as their
newly found Avathar. Theoretically, it is far easier to set up an
excellent telecommunication infrastructure in suburban and rural India
than to place hundreds of medical specialists in these places. We have
realised that the future of telecommunications lies in satellite-based
technology and fiber optic cables. Providing health care in
remote areas using hi tech is not as absurd as it may initially appear.
Could even the greatest optimist, have anticipated the phenomenal
explosion in the use of computers, in India.
What does telemedicine encompass?
Telemedicine
covers a wide range of activities. In the past it was primarily
teleradiology – the transferring of high resolution medical images, X ray
pictures, ultrasound, CT, MRl pictures, live transmission of ECGs and
echocardiograms. Today even a detailed clinical examination can be
conducted remotely.
What
are the advantages of telemedicine?
Worldwide
there is difficulty in retaining specialists in non-urban areas. The
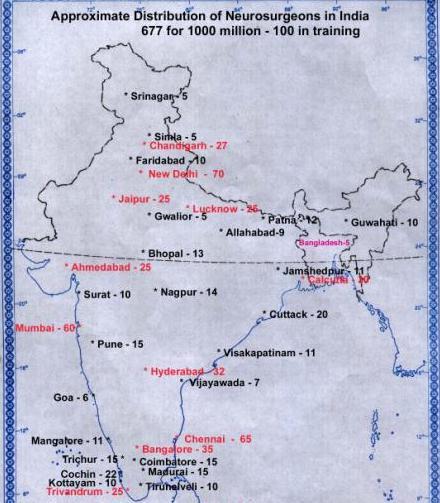
distribution of specialists in India is indeed lopsided. There are more
neurologists and neurosurgeons in Chennai, than in all the states of
North eastern India put together. Similarly tertiary care hospitals
are also concentrated in pockets with large segments of the population
having no access. The increasing availability of excellent telecommunications,
infrastructure and video conferencing equipment will help provide
a physician where there was none
before.
|
INDIA
–THE LAND OF THE
FUTURE !
65% of 1100 million will be literate by 2005
60% of rural India has access to TV coverage.
60% of rural India has access to TV coverage.
650,000 existing PCOs ® internet kiosks,.
400,000 villages already have telephone
connections.
Internet users in India 2m Dec 2001, 8.5m 2003.
Hardware, software and brain ware all
available.
|
|
|
Telemedicine
can thus avoid unnecessary travel and expense for the patient and the
family improve outcomes and even save lives. Once the “virtual presence”
of the specialist is acknowledged, a patient can access resources in a
tertiary referral centre without the constraints of distance.
Telemedicine allows patients to stay at home ensuring much needed family
support. In a large Telemedicine project in the USA 83% of patients who
would have been transferred to an urban hospital remained in their
community reducing the cost by at least 40 to 50%. This also ensures
maximal utilisation of suburban hospitals. The general practitioner in
the rural/suburban area often feels that he would loose his patient to
the city consultant. With Telemedicine the community doctor continues to
primarily treat the patient under a specialist’s umbrella. With modern
software/ hardware at either end 90% of the normal interaction can be
accomplished through Telemedicine.
The
following tables give some important facts which have to be considered
when introducing Telemedicine in India.
|
Advantages of telemedicine in India:
Doctors licensed to practice all over India,
Maximum utilisation of limited resourcesSaves
travel, time and money,
Makes Geography History!!
Enormous CME potential for GP, urban trainee and Teleconsultant,
International grand rounds, Web casting
conferences,
Motivation for computer literacy among
doctors
¯ In unnecessary referrals to
specialists,
Useful in designing credits for re
certification of doctors.
|
|
Points to be
addressed in implementing TM project:
Will faster
transmission or better image quality alter diagnosis or treatment ?
Medical Coordinators for each specialty to lay
ground rules,
Technical coordinators to identify the most
effective mode of data acquisition, compression, transfer and
manipulation at TC’s console,
Execution of pilot project within 6 months,
Collecting data over 1 year and analyzing data
over next 3 months.
|
|
Implementation
of telemedicine in India:
With software, hardware, brain ware and a
large number of doctors
licensed to practice
abroad, India could offer global Teleconsultation
at reduced
international rates.
Sophisticated extension of medical
transcription.
Marginal profits for Teleconsultation in the
metros.
TM for suburban
and rural India heavily subsidised from agencies like WHO, World Bank, Asian
Development Bank, Govt of India etc.
Successful
implementation in India = Successful Implementation anywhere in the world
|
|
Pilot study:
To evaluate acceptance– patient, GP,
Teleconsultant, public, Govt.
Identification of disciplines / diseases for
teleconsultation.
Designing appropriate need
based cost effective modules.
Training technical personnel,
GP, Teleconsultant.
Techno economic feasibility,
optimum pricing.
Limitations of Teleconsultation.
|
The Aragonda (Andhra)
Story:
As in several disciplines, the Apollo Hospitals
have been the pioneers in putting up the first modern secondary care
rural hospital using Telemedicine to provide expert care. As a
pilot project a secondary level hospital was set up in a
village called Aragonda 16km from Chitoor (population 5000). This 40
bedded hospital was equipped with a CT scan, a modern ultrasound, ECHO,
automated laboratory equipment, an incubator, automated ECG etc. A
paediatrician, a general physician and a general surgeon were available
in addition to general duty doctors.
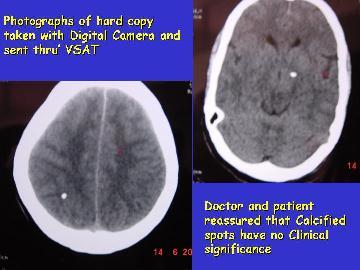
Starting from simple web cameras and ISDN
telephone lines today the village hospital has a state of the art video
conferencing system and a VSAT (Very Small Aperture Terminal) satellite
installed by ISRO (Indian Space Research Organisation). About 200 tele
consultations have been given to this village alone from specialists and
super specialists from Chennai. A specially designed software
(Mediscope) was used and the clinical history and physical findings
transferred from Aragonda. . Images of x rays and ultrasound were
scanned; compressed and sent thro ISDN lines (64 x6 384kbps). CT images
being DICOM compatible were directly electronically transferred to the
telemedicine computer for onward transmission to Chennai. Most of the
teleconsultations were initially off line – store and forward. The tele
consultant’s opinion was sent back to the primary physician. There are no
fixed hours for tele consultation – a medical officer being available at
the telemedicine unit at Chennai from 9am to 5pm. Arrangements are now
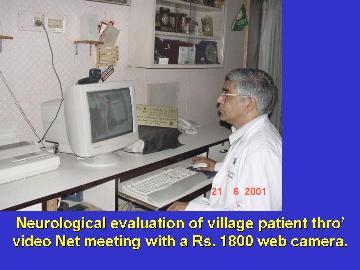
being made to provide emergency tele consultation as well. When the
tele consultant wanted to directly interact with the primary physician
and the patient, a “net meeting” was initially arranged. Later on with
availability of better infrastructure a formal video conference was held
using state of the art video conferencing equipment. . All such on line
interactions were recorded and stored. Detailed clinical “examination” of
pseudo seizures, involuntary movements, Parkinsonism, myopathy etc. was
possible. Soon an electronic digital stethoscope will be made available
so that auscultation of the heart and lungs can also be done remotely. In
almost all cases the tele consultant was able to give a definite opinion
and guide the local physician. Several serious head injuries not
requiring surgery were successfully managed in the village
hospital.
|
|
|

|
Some cases required management in a tertiary
care hospital. Details of the treatment were discussed in detail with the
patient and the family so that they were well informed and fully
prepared. These tele discussions were of considerable help. Tele
consultation was particularly useful in the follow up of already treated
patients. Interestingly the acceptance of tele consultation by the rural
patient, the sub urban doctor and the suburban community was much better
than expected. None of them were really averse to a tele consultation.
The tele consultants have also accepted this new method of interacting with
a patient. Detailed evaluation of the socio economic benefits needs to be
done.
The Sriharikota Story:
Sriharikota Space Center is an important launch
pad of the Indian Space Research Organsiation located 130 kms from
Chennai. It is actually an island. About families
live in the campus. The Health Center also provides medical assistance to
the neighbouring villages Unlike Aragonda here a virtual OP is
operational every Saturday from 10am to 1pm. 25 different specialities are
covered some every week, others once a fortnight and others once a month.
Emergency consultations on other days are also available.
Expansion Plans:
It is proposed to establish a VSAT telemedicine
link up with Port Blair in the Andaman and Nicobar Islands soon.
Connectivity has already been established with Information Centres at
Gauhathi and Calcutta. The tertiary care hospitals at Hyderabad, Delhi
and Madurai are interconnected. Tele consultation is also available to
doctors in the Middle East and other countries. Connectivity with the
Apollo Hospitals at Colombo, Dhaka, Bilaspur, Erode and others are on the
anvil.
Other uses of Video Conferencing:
The Telemedicine department of the Apollo
hospitals was the only unit from Asia which took part in the Ist Arab
International conference on Telemedicine in January 2001.
Subsequently a paper was presented from Chennai, at an International
conference on telemedicine at Upsaala Sweden in June 2001. This was an Intercontinental Live multipoint Symposium between Europe,
Africa, Asia, Australia and Americas on the topic.
“Telemedicine as a tool for a more
equitable distribution Of health care
delivery around the world”
|
Video
conferencing is an inexpensive way of
projecting the state of the art facilities available in India to a global
audience. In August 2001 the Dept of Neurosurgery Apollo Hospitals
Chennai had a two hour teleconference with the Dept of Neurosurgery
Fujitha Health University, Nagoya Japan.This international grand round
went of without a hitch. Regular conferences such as this are planned
to be conducted periodically.
This will
considerably augment the skills of all those who take part and more
important change our perspectives and help us think
|

|
|
globally.
|
Tele
conference between Apollo, Chennai & Fujitha university, Japan
|
|
|
|
|
|
Conclusion:
It is our dream that within the next few years
there will be telemedicine kiosks throughout the length and breadth of
suburban and rural India. No Indian should be deprived of a specialist
consultation wherever he/she is. This is not impossible. What is
required is not implementing better technology and getting funds but
changing the mind set of the people involved.
The first generation of
telemedicine enthusiasts should not forget that technology should be
used as a support to treat patients and not viewed as a goal in itself.
The challenge today is not confined to overcoming technological
barriers, insurmountable though they may appear.
|
|
|
It
is true that available technology still has considerable scope for
improvement. Rather the challenge is why, where and how, to implement
which technology and at what cost. A needs assessment is critical.
Due to pressure from powerful vendors the perceived needs for
Telemedicine may not conform to the actual needs. The take off problems,
facing telemedicine is legion. Telemedicine today sounds hep and cool,
but the reality may be quite different. The future however promises to be
exciting. So ladies and gentlemen hang on for the ride! Telemedicine will
be more than a roller coaster trip. The journey will well be worth the
wait.
Time
alone will tell whether Telemedicine is a “forward step in a backward
direction” or to paraphrase Neil Armstrong “one small step for IT but one
giant leap for Healthcare”.
|