|
Craniovertebral junction, and the upper cervical spine can
be approached through the neck, either through an antero-lateral or
posterior approach. But when the pathology is anterior and also requires
wide exposure on either side of mid line in the upper cervical spine, the
trans oral route helps us to reach it directly.
The transoral route is chosen ideally for extradural lesions
confined to the clivus, the C-V junction, and the upper cervical
vertebrae. The most common indication is odontoidectomy. Basilar
invagination, Rheumatoid arthritis with A-A subluxation, odontoid
fractures with A-A subluxation, Koch's spine, Chordoma, Myeloma,
Metastasis, and Lymphoma are the common problems encountered. The
intradural lesions, such as Schwannomas, Epidermoids, and Meningiomas can
also be dealt with through approach by experienced hands. Clipping of
lower and middle third basilar artery aneurysms through this route
is also possible.
Surgical anatomy:
The atlanto-axial joint is formed between the dens of the
axis and the atlas, and, one on each side, between the lateral masses of
the two vertebrae. The dens articulates with the back of the anterior
arch of the atlas by a small synovial joint.
Behind the prevertebral fascia are the median raphe between
the longus colli muscles and then the anterior atlanto-occipital membrane
which is the continuation of the anterior longitudinal ligament. The
longus colli muscles and anterior longitudinal ligament are inserted to
the anterior tubercle of C1. The longus capitis muscles run lateral to
the longus colli muscles.
The apical ligament is attached to the apex of
the odontoid process and the alar ligaments are attached
laterally on either side of it, and then to the occipital condyles.
The vertical limb of the cruciate ligament joins the
body of the axis to the foramen magnum. The transverse limb is a main
component of the cruciate ligament and attached to the posterior surface
of the arch of the arch of the atlas.. This thick ligament surrounds the
odontoid process posteriorly; between the two is a large
synovial cavity, or bursa. There is an interface between the
alar and transverse ligament. The direction of the alar ligaments is
oblique and they are located anterior to the transverse limb of the
cruciate ligament.
Posterior to the transverse limb is the slightly dark yellow
to light brown colored tectorial membrane, which is the
continuation of the posterior longitudinal ligament in front of the dura.
Surgical approaches:
We can plan the extent of exposure step by step orienting it
centrally first and extending it to the periphery as required depending
on individual requirement.
Transoral-pharyngeal approach: Click for intraoperative video
|
The patient is
positioned supine with the head extended and skull traction in place.
Alternatively, the head may be immobilized in the Mayfield frame. Some
recommend lateral position with the head immobilized in the Mayfield
frame, especially when a posterior fixation is planned in the same
sitting. This avoids unnecessary movements while positioning for
posterior fixation.
Endotracheal intubation with a flexometallic tube
positioned at the side of the mouth is adequate; some prefer routine
tracheostomy. The mouth is kept open with a gag that rests against the
upper dental arch and depresses the tongue (tonsillectomy retractor).
Several types of transoral retractors such as Crockard, Dingman,
Davis-Crowe, McGarwer etc. are available. Care is taken to ensure that
lip or tongue is not caught between the tongue blade and the teeth. A
rubber catheter should be used sometimes to retract the uvula and soft
palate. Oral irrigations with an antiseptic solution is carried out.
The soft palate may be retracted with stay stitches and
the posterior pharyngeal wall is exposed. This gives adequate exposure
for lesions at the foramen magnum and in patients with minimal basilar
invagination. Many prefer to split the soft palate to gain
better exposure; this predisposes to troublesome, though
transient, post operative nasal regurgitation in my experience.
The posterior wall of the pharynx is incised with cutting
diathermy from the roof down to C2-C3 disc or as required. Palpation of
the anterior tubercle of the anterior arch of the atlas helps to keep
the incision to midline.
The prevertebral muscles are carefully dissected from the
lower clivus, the arch of the atlas, and the C2 body on the
subperiosteal plane.
The arch of the atlas, and the dens of the axis are
drilled away. There may be some soft tissue (such as rheumatoid pannus)
behind the arch and in front of the dens which needs to be removed to
get to the dens. Lateral exposure at this level should not exceed 1.5
cm to avoid injury to the vertebral arteries. A median
corpectomy of the body of C2 (about 1 inch in diameter) down to the
C2-C3 disc level is recommended as a routine.
|
|

|

|
|
Retraction of soft palate
|
Exposing the body of C2
|
|

|

|
|
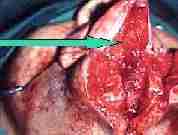
Drilling of the arch of atlas
|
Excision of soft
tissue behind arch
|
|

|

|
|
C2 corpectomy
|
Drilling of odontoid
|
|

|

|
|
Transverse lig.
after odontoidectomy
|
Pharyngeal closure
|
|
Removal of the dens will expose the transverse limb of the
cruciate ligament and apical ligament. This may be removed along
with the lower most tip of the clivus for presumed better
decompression as recommended by some. This step is better avoided in my
opinion and adds to instability.
Additional extradural/ intradural pathology is dealt with as
required.
The pharyngeal wall may be closed in a single layer with
absorbent suture material. The palate is closed in a single layer as
well, if it had been split.
Post operatively, nasogastric tube feeding is established
for a week and the patient is mobilized with a 'Philadelpia'
cervical collar to restrict the atlanto-axial joint movements.
Extended approaches:
Extended transoral approaches include maxillary osteotomy,
mandibulatomy and other skull base approaches.
Bilateral LeForte maxillary osteotomy can be
done through a trans oral sulcus incision and the maxillae can be pushed
down as a single piece and by resecting a part of nasal septum we can
have adequate exposure superiorly.
If necessary we can further split the maxilla in the center and swing
both the halves of maxillae on either side outward and a wide access can
be achieved.
|
This approach is
particularly useful for lesions of the upper and midclivus. The roof of
naso pharynx is another area, which is difficult to reach, and trans
oral route combined with splitting the maxilla gives wide access.
|

|

|

|
|
Leforte osteotomy
|
Osteotomy completed
|
Hard plate split
|
If access is required inferiorly a mandiblotomy may
be added. The mandible can be split in the mid line or para sagittaly and
the floor of mouth and tongue can be split in the mid line .The
mandibular halves can be swung outwards gaining excellent exposure. No
significant post operative functional or esthetic problems are expected.
|

|

|

|

|
|
Mandible split
|
Tongue split
|
Floor of the mouth split
|
C2 Tumor bulge
|
|
|
|
|
|
|

|

|
|

|
|
after excision
|
Mandible closure
|
Tongue closure
|
Skin closure
|
This approach is useful for a radical excision of upper
cervical spine lesions with lateral extensions.
In the same way if the lesions are to one side of mid line,
we can combine the central oral exposure with maxillary osteotomy of one
side. If further superior access is required we can include the nose,
floor and lateral walls of orbit along with this as zygomatico maxillary
osteotomy. Care must be taken not to jeopardize the vascularity of the
maxillary segment.
Stabilization:
Most surgeons recommend some form of stabilization either in
the same sitting or as a second stage. Another school feel that
stabilization is not required in selected patients.
Absolute indications for stablization are
History of precipitating trauma,
Symptoms suggestive of instability, such as suboccipital
pain (occipital neuralgia), and worsening deficits on neck flexion,
Radiological suggestion of instability,
Patients under 40 years of age,
Post operative suboccipital pain (occipital neuralgia).
|
Posterior
stabilization is widely practised; occipito cervical wiring or plating,
atlanto-axial sublaminar wiring, use of Hartshil frame or
interpedicular screws are in common use. No one is superior to another;
adequate bone grafting is a must.
Anterior fixations are becoming popular and avoids another
incision and procedure. Infection is a potential threat.
|

|

|

|
|
|
post. wiring
|
post. plating
|
Hartshil frame
|
Postoperatively the patient may be mobilized with a
'Philadelphia' collar or an 'Halo' frame for about 6 weeks.
Complications:
Transient nasal regurgitation is
common; retraction of the soft palate instead of splitting reduces this
risk. Continued nasogastric tube feeding is recommended to tide over this
problem.
Dural tear may lead to CSF leak and
meningitis; careful drilling and use of fine up-cutting punches help to
prevent this. A continuous lumbar CSF drainage in a closed system
for a week will help seal off the leak. If persists, an occult
hydrocephalus should be thought of.
Pharyngeal wound dehiscence is
rare; healing is surprisingly good in the oral cavity. Continued
nasogastric tube feeding is indicated untill satisfactory healing.
Snapping of posterior wiring has
been reported and requires refixation.
Oral edema may be avoided with large
dose of dexamethasone at the time of incision and topical application of
steroid cream at the operated site; may warrant a tracheostomy.
Infection is a dreaded problem; may
require removal of fixation system and nursing the patient with a Halo
frame of skull tongs for 2-3 months.
The outcome depends on the preoperative neurological
status, duration of illness, and the nature of the pathology.
|