|
The history of development of surgery for acoustic neuroma
dates back to Cushing and Dandy.
Various surgical approaches are employed.
They are: suboccipital, trans labyrinthine, and middle fossa
approach.
The patient's age, hearing status, tumor size, and above all,
the surgeon's preference decide the approach. On occasions, a combination
above approaches can, effectively, be employed.
1) Suboccipital (retrosigmoid transmeatal) approach:
It
is the most widely used approach.
Anatomy of the CP angle:
The CP angle or fissure is V shaped and is formed by the
folding of petrosal surface of the cerebellum lateral side of the pons and medial
cerebellar peduncle. The floor of the space is formed by medial peduncle.
The cerebello medullary cistern is situated between the
cerebellar tonsils and medulla and communicates with the CP angle
cistern near the foramen of luschka. The trigeminal, the abducent, the
facial, the vestibulocochlear and glasso-pharyngeal arise between the
superior and inferior limbs of the CP angle.
The internal acoustic meatus has a width of 9 to 10mm and
height of 3 to 6mm. The internal auditory canal has a length of 6 to 7mm
and the height of 3 to 7mm. The falciform or transverse
crest divides the meatus into the superior and
inferior portion.
There are 4 nerves at the IAM-the facial, the cochlear, the
superior and inferior vestibular nerves. The facial nerve and the superior
vestibular nerve are superior to the crest with the facial nerve
placed anteriorly. The cochlear nerve and the inferior vestibular nerve are
in the inferior portion of the crest with cochlear nerve
anteriorly.
The facial nerve arises from brainstem near the lateral end of
the ponto-medullary sulcus, 1 to 2 cm anterior to the point where
vestibulo-cochlear nerve enters the brainstem at the lateral end of the
same sulcus. The facial nerve arises 2 to 3 cm above the emergence of the
superior most rootlet of lower cranial nerves from the
brainstem. The intra cistern length of the facial is 9 to 26mm.
The vestibular-cochlear nerve enters the brainstem 13 -
17 mm from the midline and
its intra cistern length is about
14.9 mm. While entering the brainstem, the cochlear part is lateral
most and the superior vestibular the most medial with inferior
vestibular in between.
The length of the trigeminal nerve in the CP angle and the
posterior fossa is 12.3mm for the sensory root and 14.1mm for the motor
root. It exits from the posterior fossa through the dural opening situated
at the anterior end of the medial surface of the tentorium cerebelli. The
superior petrosal sinus is closely associated with the nerve and superior
cerebellar artery also forms a close relationship to the
nerves.
The abducent nerve emerges from the brainstem approximately
3.9mm lateral to midline. The 9th and 10th cranial nerves merge caudal to
pondomedullary sulcus. The anterior inferior cerebellar artery is closely
related to the facial and vestibular cochlear nerve.
Internal auditory artery, the recurrent
perforating arteries and the subarcuate artery are the branches
of AICA. The superior petrosal vein (Dandy's) is the principle draining
vein of antero-lateral posterior fossa structure. The vein is 1 to 2mm in
diameter. The inferior petrosal vein courses along the vagus nerve.
Pathological anatomy:
Schwannomas arise most commonly from the vestibular nerve
(80%), occasionally from the cochlear (5to 7%). The inferior vestibular
nerve is involved in 70%, superior vestibular in 20% and cochlear nerve in
10%.The origin of the tumor is from junctional (Obersteiner
Redlich) zone where the central and peripheral myelin meet. This zone is
situated at the region of IAM or within the internal auditory canal. The
tumor grows initially within the canal and thereafter, extrudes into the CP
angle. Inside the petrous bone, the tumor
may compress the cochlear component
of the nerve or the labyrinthine artery, causing
sudden severe hearing loss. Growth of the tumor in to the
CP angle leads to the anterior displacement of the facial and cochlear
nerve. The relationship of the tumor to the
vestibular cochlear nerve varies. In about 50%, the
nerve fibers are intimately involved with the tumor, making separation
impossible. In 40%, though the nerve is in the form of bundle initially, it
becomes adherent and a part of the tumor capsule making
functional preservation impossible, and in 10%, uninvolved portion of the
nerve maintain anatomical integrity. Anatomically the
last group present with preservation of hearing and
in this group, the vestibular cochlear nerve is displaced
inferiorly in 80%,anteriorly in18% and posteriorly.
Depending on the direction of growth of the tumor, the
facial nerve may be displaced anterosuperiorly or
anteroinferiorly. The facial nerve may run one of 4 courses around the
acoustic neuroma. The nerve runs anterior to the tumor in 70%, superior in
about 10%, posterior in 7% and inferior in 13%.
The position of the facial nerve is most constant at the
lateral end of the IAM. The nerve may be anatomically distorted by the
tumor in about 2/3rd of cases, the nerve maintains the shape of a thin
bundle, while in about a 3rd of cases, and the nerve fibers are splayed
over the tumor capsule. Since the tumor arise from outside the CSF space,
it pushes the lateral layer of the arachnoid inwards till it comes into
contact with the middle layer. The double layer thus formed contains the
important vessels and nerves of the CP angle.
Management of pre-operative hydrocephalus:
Patient with acoustic neuroma with obstructive hydrocephalus are
shunted using Chabbra medium pressure tube as a first stage. This helps in
reducing the intracranial tension, and prevents post operative CSF leak due
to increased intracranial pressure. This can be done few days earlier to
surgery.
Pre-operative preparation:
Pre-operative steroids are advocated by
many. I have practiced giving steroids
only per-operatively and post-operatively for a short
duration. The previous night of surgery, broad spectrum antibiotic is given
along with sedation.
On the day of surgery, 45 minutes
before surgery, premedication is given using
Pethidine 100gms IM and Atropine 0.6 mgs I.M.
At the time of inducing anesthesia, another dose antibiotic
is given I.V. Minimum 3 IV lines
are maintained, of which, one is a
central line (CVP). Indwelling Foley's catheter is inserted and
crepe bandage applied for both lower limbs.
Monitoring of the patient:
Continuous ECG, PaO2 NIBP monitoring is done.
Electrophysiological monitoring of facial nerve function if available is
useful.
The stethoscope with a long tube is attached and fixed with
dynaplast to the chest over pre-cardial region for auscultation of
the heart by the anesthetist for any air embolism
is practiced in our unit.
Positioning:
Though various positions are employed, such as semi sitting,
lateral or sitting position, surgeon's preference should be taken into
consideration for appropriate positioning of the patient. I usually do all
patients in sitting posture with head fixed with 3 pin fixations.
Both legs should be kept slightly flexed at the knee level as
keeping them straight may cause stretching of sciatic nerve and
post operative sciatic pain.
Adequate side support on the sides with pillows and one pillow
just below the knees are kept to make the position comfortable to the
patient and support the patient adequately in sitting position.
It should be made sure that no part of the body comes in
contact with any metallic part of the operation table as this may cause
electric shock/electric burn while using monopolar diathermy.
Also due attention paid while flexing the neck under
anesthesia - 2 fingers should be kept between the
chin and the chest and the head is turned to the ipsilateral side of
the tumor for about 20 to 30 degrees, so that, when the surgeon
approaches the tumor, his vision is in line with the tumor/brainstem.
Those elderly patient who do not tolerate sitting posture due
to fall in BP, surgery can be done in lateral position. Before making the
patient sit up slowly, about 1500cc of fluids should be given IV so that
there is no fall in BP while making the patient sits up. Adequate time
should be taken to make the patient sit up with periodical BP monitoring.
Iodine solution is used liberally. Initially iodine scrub
solution is used and the operating site is scrubbed for a minimum period of
5 minutes. This is followed with another preparation with 10% iodine
solution.
It is always advantageous to have an accessibility to the
ventricle post operatively and also for patients who undergo surgery in
sitting posture to prevent pneumocephalus. It is better to have a burr hole
before proceeding for tumor excision. A 2 cm horizontal skin incision is
made 7 cm above and 3cm lateral to the EOP on the ipsilateral side of the
tumor. The burr hole is done and the dura is opened after cautery in a
cruciate manner. Pia is also cauterized and opened. Hemostasis achieved and
the wound is closed in single layer.
|
Subsequently a vertical retromastoid skin incision is made
from the level of EOP down up to C2. The suboccipital muscles and fascia
are incised and are carefully separated from their attachment to the bone
by using periosteal elevator and electrocautery. While
separating from the bone, there are chances for air
being sucked in through emissary veins and this
may cause air embolism. Hence, periodically bone wax is applied to the
bone to obliterate the opening, and anesthetist is requested to
keep a watch on the heart sounds for early
detection of air embolism. Subsequently a burr hole is made
just behind the mastoid and converted into craniectomy by further
nibbling. A craniotomy can be used to make a bone flap which can be
replaced later. The craniectomy is done such that superiorly the
transverse sinus is visualized, laterally the sigmoid sinus, inferiorly
as much as possible to expose the floor of the posterior fossa.
|
|
After adequate relaxation of the cerebellum, it will be
possible to retract the cerebellar surface easily. A broad lint or soft
roll or thin rubber sheet from the gloves may be used to cover the
cerebellar surface and the retraction to the cerebellum is gently applied
to expose the surface of the tumor.
Most
often, there is thin layer of arachnoid seen covering the tumor. The good
result of the surgery is achieved by maintaining the integrity of the
arachnoid layer. As long as it is maintained, it is easy to protect the
nerves and vessels encountered.
|
The arachnoid over the tumor should not be cauterized as it
may become adherent to the tumor surface and separation may be difficult
and the arachnoid layer will be lost. Arachnoid layer is opened.
Once the tumor is exposed adequately using Leyla retractors,
usually two retractors one above and one below covering the cerebellar
surface, the capsule of the tumor should be opened. The opening should be
made horizontally so that one can avoid injuring the nerves
going across the tumor anterosuperiorly. Since the space may be inadequate
for manipulation of the tumor, debulking of the tumor should be done as
much as possible so that further dissection is made easy.
|
|
Debulking may be done using bipolar coagulation, scoop or CUSA
if available. While using CUSA, one should be careful, not to try to debulk
the tumor too fast or take a CUSA probe too much anteriorly as it may
suck in the facial nerve. If one is careful, then the CUSA can be used
advantageously and reduces a lot of operating time.
After adequate debulking using fine dissectors, it will be
possible to separate the capsule from the arachnoid.
Most of the time, the tumor is not adherent to the brainstem.
But the arachnoid layer can be missed. This is the situation where
difficulty will be encountered in separating the tumor from the brainstem.
Also small nubbin of the tumor may be indenting the brainstem and there
will be difficulty in separating such nubbins from the brainstem, if the
arachnoid layer is not intact. Also if arachnoid is breached, it will be
difficult to separate and preserve the veins going into the brainstem.
Hence one has to be careful in separating the arachnoid layer and
preserving it intact.
After debulking the tumor, the capsule of the tumor is lifted
from below upwards exposing the lower cranial nerves. The nerves can be
easily separable from the tumor capsule by fine dissectors and protected by
covering with lint pieces. At this stage, one can see whether there is any
blood supply from the vertebral to the tumor or from AICA. Large branches
from inferior cerebellar artery are sometime embedded in the tumor capsule
which can usually be dissected free by dividing the small branch directly
supplying the tumor.
Subsequently the dissection carried out superiorly separating
the greater petrosal vein from the tumor surface. Sometimes it may be
necessary to cauterize and cut this vein and it does not cause any undue
sequelae. While separating the arachnoid superiorly, the trigeminal nerve
will come into view. It can easily be identified by its thickness. This
could easily be separated from the tumor surface, using fine dissectors.
Periodical debulking and excision of the capsule is done so
that adequate space is created and the dissection is made easy.
While separating the tumor medially from the brainstem, the
DREZ zone of the V, VII, and VIII nerve complex will be encountered.
|
By following the VII and VIII nerve complex from the DREZ,
it is possible to identify the nerve which is most often anteroinferior
to the tumor.
There are situations where the nerve may be encountered
anterosuperiorly or very rarely posteriorly. One should be aware of the
different variations of the course of the nerve.
After adequate debulking, the nerves are traced to the IAM.
Here the dura over the IAM is incised and the IAM is opened
to expose the tumor. Usually bone is removed not more than 10 mm
laterally or else there is a risk of entering into the labyrinthine.
At this stage, fine dissectors are used to debulk and tease
the tumor from the nerve fascicles. The tumor however comes off easily
and total excision of the tumor can be achieved.
Very rarely, one may have to leave a small bit of the tumor
over the nerve if the tumor is firmly adherent and the removal may cause
damage to the facial nerve. After adequate removal, the whole anatomy of
the CP angle is well visualized and one should make sure
about absolute hemostasis.
|
|
|

|
|
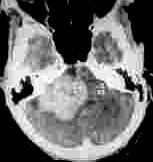
Pre-op.
Rt. ANF-CT
|
Post-op.
Rt. ANF-CT
|
|

|

|
|
Pre-op.
Lt. ANF-CT
|
Post-op.
Lt. ANF-CT
|
|
I do not use gelfoam over the brainstem or the nerve
roots to get hemostasis as they may cause post-op complications.
After hemostasis, a bit of fat and fascia are kept within IAM to
prevent CSF leak. Then the dura is closed using 5.0 prolene. If dura is not
closed, it is better to harvest pericranium or fascia lata and cover the
dural defect to prevent CSF leak post operatively. The bone bits collected
during craniectomy and bone dust while doing burr hole are sandwiched
between split gelfoam and replaced extradurally and wound is closed in 4
layers. A Ryle's tube is passed before extubation and the tube is kept for
few daystill the swallowing is tested.
Post operative management:
Constant vigil is kept over patientís conscious level. If the
level of conscious deteriorates, immediate CT scan is done to rule out post
operative hematoma which may need immediate evacuation.
Occasionally CSF leak may occur, if the dura is not completely
closed leaving behind a small hole which may act as ball valve. If
dura could not be closed it is better to leave the dura totally
open and not to close partially. This will prevent CSF leak. Sometime,
there may be CSF leak due to local collection which may stop in a day or
two.
With those patients who have not undergone shunt surgery, one
has to keep an eye for the development of hydrocephalus which may
need shunting.
Meningitis though not common, may develop and needs immediate
lumbar punctures to drain CSF and broad spectrum antibiotics
coverage. Post operatively, all patients are kept in tapering dose of
steroids (4mgs of Dexamethozone twice daily for 3 days and
gradually reduced over a period of three days and then stopped).
Even, if facial nerve is preserved anatomically, there is
likely development of facial nerve paralysis. This may need torsorraphy to
protect cornea and prevent exposure karatitis.
In elderly patients, active chest physiotherapy and early
mobilization are necessary to prevent DVT and pneumonia.
In our experience, 95% of the tumor can be excised totally and
another 5% radically. Facial nerve preservation is possible only in 60 to
70% of the cases as the tumors encountered are very large and the facial
nerve complex is splayed out. In these circumstances, it is difficult to
preserve the facial nerve anatomically.
Translabyrinthine approach:
This
approach, discussed elsewhere,
may be used in larger tumor
with no hearing. The goal is to preserve the facial nerve.
Middle fossa approach:
A small group of surgeons recommend a
middle fossa approach to
tumors of the IAC (intracanalicular) or those with no more than 1cm of CPA extension. The goal is
to preserve hearing.
A thorough knowledge of temporal bone is mandatory.
The
patient is positioned in the park bench or true lateral position with the
head fixed in Mayfield clamps, and the surgeon is seated above the
patient's head.
A
small subtemporal craniotomy is made just above the ear.
The
dura is separated from the temporal bone. The lower marigin of the
craniotomy should be in line with the middle fossa floor.
Extradural
dissection is carried out, after mannitol diuresis to minimize the temporal
lobe retraction. Lumbar CSF drainage at this stage helps.
The
arcuate eminence, which is the guide to the superior semicircular canal,
and must be identified. The foramen spinosum is the anterior limit of the
exposure. Medial limit is the superior petrosal sinus.
The
greater superficial petrosal nerve, as it exits from the facial hiatus on
the floor of the middle fossa, and the lesser petrosal nerve should be
identified. The greater superficial petrosal nerve leads to the geniculate
ganglion, and the facial nerve.
Internal
auditory canal (IAC) is exposed following the greater superficial petrosal
nerve to the geniculate ganglion.
The
petrous bone is drilled over the arcuate eminence and the IAC is
skeletonized. Bone removal should not injure the superior semicircular
canal, labyrinthine segment of the facial nerve, or cochlea. Extensive
skeletonization of the IAC is carried out. Medially, it is possible to
expose 270 degrees of IAC and posterior fossa dura can be uncovered for
approximately 2 cm.
'Bill's
bar', a vertical crest at the lateral end of the IAC, arising from the
transverse crest is a key land mark. It separates the anteriorly situated
facial nerve from the more posteriorly situated superior vestibular nerve.
The facial nerve is identified, and protected.
The
dura is opened parallel to the long axis of the IAC following bone removal.
The
tumor is removed in piecemeal.
The
dura is closed watertight, and the bone flap is replaced and fixed.
Complications
include
seizures, injury to vein of Labbe, and injury to cochlear or facial nerves
or the inner ear.
|