|
Dermoids and
epidermoids are the result from an abnormality of surface ectoderm, and
invariably associated with one or more mesodermal malformations, such as,
those involving the vertebrae.
Similarly,
neuroenteric cysts are due to an endodermal malformation.
Other developmental cysts, including the Arachnoid cysts
are discussed elsewhere.
EPIDERMOIDS:
Epidermoid cysts constitute
approximately 0.2 to 1.8% of all intracranial tumors and less than 1% of
all intraspinal tumors. Cranial sites outweigh spinal sites by 14:1.
Although these lesions are congenital, patients are usually not
symptomatic until they are aged 20-40 years.
Pathology:
They are benign
congenital lesions of ectodermal origin. Epidermoid cysts represent nests
of cutaneous tissues misplaced during embryogenesis and found along lines
of ontogenic neurocutaneous differentiation. These ectodermal inclusions
occur between 3rd & 5th Weeks of
embryonic life. This inclusion can result in heterotopia of these
elements. The median location of these tumors can be explained by the
separation of neuroectoderm & its cutaneous counterpart which occurs
dorsally along the midline. Laterally situated lesions may result from
inclusion of ectoderm at a later stage of embryogenesis, especially
during the formation of secondary otic and optic cerebral vesicles.
In
the
spine these lesions are usually associated with spinal dysraphism
. Acquired epidermoid cysts in the lumbar area are due to repeated lumbar
punctures or incidental formation of a skin pocket by suturing.
Grossly, they are well
circumscribed, smooth or lobulated, encapsulated friable lesions with a characteristic glistening pearl like
sheen. Typically, the epidermoid contains white, flaky, kertinous debris.
|
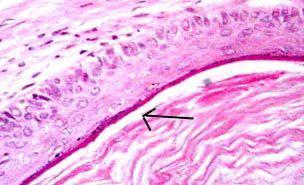
Histologically, they appear
as an internal layer of keratinized, stratified squamous epithelium
with a whitish fibrous capsule; these features account for the term
pearly tumor. They tend to slowly enlarge as epithelial cells
desquamate, with the formation of keratin and cholesterol crystals in
the center of the lesion.
Approximately, 25% are situated intradiploically
in the skull or spine. The vast majority of epidermoids are intradural
The most common locations are within the cerebellopontine (CP) angle,
parasellar region,pineal region and middle cranial fossa.
|
|
|
|
Epidermoid
cyst (H&E): The cyst is lined by epidermal layer(arrow)
(keratinized, stratified squamous epithelium).
|
|
The
CP angle is the most common site for epidermoids. Of all CP angle masses,
epidermoids are the third most common after vestibular schwannomas and
meningiomas. Occurrences within the ventricular system, brain parenchyma,
and even the spinal cord, have been reported.
At
diagnosis, epidermoids usually insinuate within the sulci and cisterns,
and they may engulf cranial nerves and blood vessels.
Clinical
features:
Clinical
features depend on the site of location, and indistinguishable from any
other mass lesion. The average age of presentation is 35 years with a
female predominance. They grow linearly, similar to normal skin, and thus
have an insidious onset. Rarely, there may be features of aseptic
meningitis, caused by leakage of the debris into the subarachnoid spaces.
Spinal
epidermoids are usually associated with vertebral anomalies.
|
Imaging:
Skull
radiographs
may reveal a lytic lesions with well-defined sclerotic borders. Rarely
the epidermoids show calcifications.
CT
and MRI
are both helpful in diagnosing epidermoids. Although CT findings may be
nonspecific, MRI findings are reliable in diagnosis.
|
|
|
|
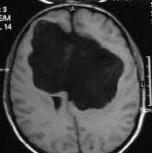
Bifalx epidermoid- MRI
|
|
Epidermoids
lesions usually have the same attenuation as that of cerebrospinal fluid
(CSF); this characteristic makes their differentiation from arachnoid
cysts difficult; however, the margins of these lesions are typically
lobulated and may contain fine linear strands. They may also envelope
rather than displace surrounding structures such as cranial nerves. Enhancement
is rare, but can sometimes be seen around the margin of the tumor.
Differentiation from CSF filled
lesions can be made on diffusion weighted MRI because these lesions have
diffusion characteristics of solid tissue whereas the diffusion
characteristics of an arachnoid cyst are similar to CSF. These lesions
also show significant magnetization transfer on magnetization transfer
sequences whereas arachnoid cysts show no magnetization transfer.
The contents of the cyst may also
rarely demonstrate high signal on T1-weighted sequences similar to a
lipoma or dermoid. Because the latter two lesions contain fat chemical
shift artefact will be present whereas an epidermoid contains no fat.
This distinction can also be made by applying a fat saturation sequence
which will leave an epidermoid unchanged whereas the high signal from fat
will disappear if the lesion is a dermoid or lipoma.
Proton
density–weighted and then fluid-attenuated inversion recovery (FLAIR)
images were first used to differentiate epidermoids from arachnoid cysts.
These sequences demonstrate epidermoids as being hyperintense relative to
CSF.
Now,
diffusion-weighted imaging can be used to differentiate these entities,
because epidermoids have markedly restricted diffusion and, therefore,
high signal intensity on the diffusion-weighted trace images. The free
water in arachnoid cysts has low signal intensity.
Diffusion-weighted
images are helpful in assessing residual epidermoid tumors after surgical
resection.
Contrast
enhancement suggest a malignant epithelial component.
Management:
Treatment
is surgical removal. Asymptomatic, incidentally discovered cysts need not
be removed, but followed up regularly. Gross total resection is the goal,
but because the cysts can be very adherent to adjacent blood vessels,
total excision is not always possible. The capsule is the living portion
of the tumor, and viable portions that remain will likely regrow, but at
such a slow rate that the tumor may not become symptomatic during the
patient's life time. Spillage of the contents must be prevented, as they
may cause severe chemical meningitis.
There
is no role for radiotherapy or chemotherapy.
The
tumor marker CA 19-9 is positive in many cases and may provide a means of
follow up for the residual and recurrence.
DERMOIDS:
They
are also been described as hamartomas, hamartomatous tumor, dermoid
cystic tumor, cystic teratoma, congenital cyst of the spine, spinal
dermoid cysts, subcutaneous cysts.
Dermoid cysts can be
intracranial, intraspinal, or perispinal.
Pathology:
|
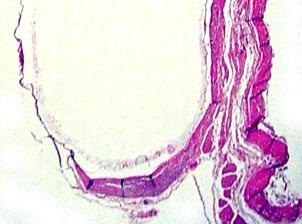
Dermoid cysts are true
hamartomas. Dermoid cysts are a result of
the sequestration of the skin
along the lines of embryonic closure.
They are benign and demonstrate
both dermal and epidermal elements.
The tumor is covered by a thick
dermis like wall that contains
multiple sebaceous glands and
almost all skin adnexa. The dermoid
contents
include cheesy, granular material. Hairs and large amounts of
fatty masses cover poorly to
fully differentiated structures derived
from the ectoderm. The dermoid cyst also contains
pilosebaceous
units with
hair shafts and sebaceous glands. Dermal elements may
be found
in only a small part of the capsule, and the rest of the cyst
wall may
closely resemble an epidermoid cyst.
A dermal
sinus tract may connect the cyst to the skin surface,
especially
when the cyst is located in the posterior fossa,
or spinal
canal.
|
|

|
|
Dermoid cyst (H&E): The cyst
shows both epidermal and dermal (adnexal structures-arrow)
lining.
|
|
Clinical features:
Symptoms depend on the location
and are, usually, that of any other mass lesion.
They are more commonly seen in
the spine than the brain.
When found in the brain, they
tend to be in the midline.
Dermoid cysts are usually seen in
children, unlike the epidermoids which are seen in adults and can
be associated with episodes of aseptic meningitis, due to leakage
of its content.
|
In
some patients, spinal dermoid cysts, especially those connected to
dermal sinus tract, lead to severe neurologic complications such as
secondary spinal subdural abscesses caused by the spread of the
infection in the dermoid cyst.
Imaging:
CT
and MRI
are helpful in making the correct differential diagnosis of dermoid
cysts. 20% of the dermoids calcify.
MRI
is particularly helpful in diagnosing intracranial or intramedullary
dermoid cysts and in assessing the dissemination of fatty masses or
droplets and also the associated sinus tracts. MRI is helpful in
planning surgical procedures and in assessing therapeutic success. They
are usually hyper dense on both T1 and T2, and more solid than
epidermoids, they are less likely to insinuate between neurovascular
structures and tend to demonstrate more of a local mass effect with no
edema.
Management:
|
|

|
|
Spinal dermoid-MRI
|
|
Surgical
excision is the treatment of choice in any localization, and the excision
is easier than in an epidermoid. Several possible complications of
spontaneous or posttraumatic rupture and surgical procedures have been
described. In patients with a ruptured spinal dermoid cyst, fatty
droplets can disseminate in the cerebrospinal fluid or in a dilated
central canal of the spinal cord. In other patients, subarachnoid
and ventricular fat dissemination can occur after the cerebellopontine
angle dermoid cyst is resected. Spinal subdural abscesses are a
possible complication because of the bacterial infection of spinal
dermoid cysts in a dermal sinus tract.
As
in epidermoids, the tumor marker CA 19-9 is positive in many cases and
may provide a means of follow up for the residual and recurrence.
NEUROENTERIC CYSTS:
(also known as enterogenous cysts,
endodermal cysts, archenteric cysts, gastrocystomas, intestinomas, cystic
teratomas, foregut cysts)
They represent approximately 0.7% of
tumors and 16% of cysts in the CNS. 5% of patients with Klippel-Feil
syndrome and vertebral fusion abnormalities may have enteric cysts.
During normal development, the
neuroenteric canal closes and the notochord separates from the primitive
gut in the third week of embryonic life. It is proposed that during the
same period, a transient adhesion occurs between the neural ectoderm and
endoderm, or a communication develops along the neuroenteric canal.
When such a developmental abnormality persists because of the
incomplete separation at this adherence or remnant canal, the cyst
forms. They are often associated with developmental defects of the
overlying skin and/or vertebral bodies.
Enterogenous cysts of the central
nervous system occur most frequently in the spinal canal, especially in
the lower cervical and upper thoracic(42%) regions with intradural,
extramedullary location. Intracranial neurenteric cysts are typically
intradural, extra-axial posterior fossa masses.
|
They are benign epithelial
lined cysts, with the lining resembling that of the alimentary canal.
They are well delineated, thin walled, fluid containing masses. These cysts are similar to
Rathke cleft cysts and colloid cysts at histologic and immunochemical analysis. The location of
these lesions on images is an important distinguishing feature. A Rathke cleft cyst is usually sellar or
suprasellar, whereas a colloid cyst is related to the anterior wall of the
third ventricle adjacent to foramen of Monro. Neurenteric cysts have been reported in the
cervical, thoracic, and lumbar portions of the spinal canal, the posterior cranial fossa, the suprasellar
cistern and the
anterior cranial fossa.
The cyst wall is composed of
fibrous connective tissue with an underlying epithelium that resembles
gastrointestinal or respiratory tract mucosa (unlike the arachnoid cyst
which is lined with meningothelial cells).
Cyst contents vary from
colorless, transparent fluid resembling CSF to milky or mucinous like
secretions. Occasionally they can have fistulous connection with
similar mediastinal, thoracic or abdominal cysts, thus supporting an
endodermal origin of these cysts.
|
|
|
|
Enteric
cyst (H&E): Cyst lined by simple columnar and cuboidal
epithelium.
|
|
|
Their intracranial occurrence
and the lumbar spine are rare sites.
Between 85% and 90% are
midline; most are located ventral to the spinal cord or brain stem.
Spinal variety is more common in men, whereas the intracranial ones are
commoner in women. They may be asymptomatic lesions that are
discovered incidentally; the larger ones present with gross
ataxia, nystagmus, visual symptoms and cranial nerve palsies.
Pain and myelopathic symptoms are common in spinal lesions;
septic or chemical meningitis may occur. They may present prenatally up
through adulthood. In adults the presentation is slow and insidious.;
progession is rapid in children.
CT scan reveals a well
delineated, non enhancing, noncalcified lobulated mass that is
typically hypodense compared to adjacent brain parenchyma. It may be
difficult to defferentiate from arachnoid cyst on CT.
MRI signal varies with cyst
content; most lesions are iso to mildly hyperintense compared
to CSF on T1-weighted images
and moderately hyperintense on proton density and T2-weighted
sequences. Spinal ones are, invariably associated with vertebral
anomalies.
Differential diagnosis includes
arachnoid and neuroepithelial cysts, epidermoid cyst, cystic schwannoma
and inflammatory cysts such as cysticercosis.
|
|

|
|
Cervical neuroenteric cyst-MRI
|
|
Treatment is surgical
excision. The goal is complete excision, which is not always possible.
Simple aspiration, cyst wall
marsupialization, or cysto-subarchnoid shunt may be employed when total
removal is not possible. There is no role for radiotherapy or
chemotherapy.
|