|
Extradural hematoma (EDH) can be the most satisfying case
for a neurosurgeon and constitutes a major source of preventable
mortality in the head injured.
Epidemiology:
It occurs in all age groups, but mostly in under the age of
40 years and commoner in males. It is the most common post-traumatic
intracranial hematoma in children and follows SDH and ICH in adults. 10%
of fatal injuries in Glasgow autopsy series, 1-4% of imaged
craniocerebral trauma, and less than 2% of admitted craniocerebral trauma
have EDH.
Aetiology:
It is the result of an impact injury most common in
road traffic accidents, assaults, and fall from a height. Occasionally,
it may present as a post operative event or as a result of bleeding from
a dural AVM.
Pathophysiology:
The potential extradural space needs to be stripped off the
inner table before the meningeal vessels bleed. In children under 3 years
and in the older age group, the dura is adherent to the inner table and
hence the EDH is less frequent.
In more than 50% of EDHs, the source of bleeding is a
ruptured middle meningeal artery. In 33%, it is a ruptured middle
meningeal vein. The rest is from venous sinuses and diploic veins. The
extravasated blood separates the dura from the bone, leading to
detachment of further vessels thus aggravating the bleeding; the
stripping do not cross the suture lines. Over 80% of them are associated
with a fracture.
In 67%, the involved site is temporo-parietal region, and in
about 10%, the site is frontal. Occasionally it is bilateral.
Posterior fossa EDHs are uncommon, but the
clinical deterioration is rapid. A fracture at the region of transverse
sinus or a diastasis of the lambdoid or occipito-mastoid suture should
alert the surgeon. A collection of 15ml of blood in the subtentorial
space results in severe functional disturbance. Obstructive hydrocephalus
is an ever present possibility.
Clinical features:
|
The volume is not always directly proportional to the
severity of the clinical symptoms. 25 ml of hematoma is considered
significant. The clinical picture depends on location, rapidity
of hematoma formation, associated intradural and other injuries, and
internal decompression through fractures (blood & CSF
leakage).
The classical triad of head injury with lucid interval,
ipsilateral mydriasis and contralateral paresis occurs only in 18% of
cases and mainly in hematomas of the parieto-temporal hematomas.
Often, the clinical picture is a combination of the above.
There are no definite symptoms of epidural hematomas. The
clinical course may the same in acute SDHs, ICHs, and temporal and
frontal contusions.
|
|
In acute
EDHs, the frequency of the clinical presentations is as follows:
|
|
hyperacute
course (up to 10 hours)
|
10%
|
|
acute course
(up to 24 hours)
|
38%
|
|
short LOC
followed by lucid interval (classical type)
|
18%
|
|
irritability,
headaches, nausea
|
84%
|
|
GCS<7
from the onset with progressive deterioration
|
31%
|
|
ipsilateral
anisocoria
|
50%
|
|
contralateral
anisocoria
|
4%
|
|
contralateral
hemiparesis
|
62%
|
|
ipsilateral
hemiparesis (kernohan's phenomenon)
|
3%
|
|
|
In subacute or chronic types, the lucid
interval may last for days and weeks.
In children, seizures, vomiting, irritability,
lethargy are common. The onset of symptoms may be delayed, but
deterioration may be rapid. Fracture is uncommon. Blood volume lost to
the extradural space in an infant may be enough to produce a clinical
picture of shock.
|
Investigations:
X-rays of the skull may reveal a
fracture, suggesting the site of the EDH.
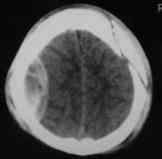
CT scan is the investigation of
choice. The minimal volume required for visualization in CT is about
25ml. Initial CT may be negative in about 30% of cases. The hematoma is
seen as a biconvex, hyperdense, nonenhancing extraparenchymal lesion.
Heterodensity (Glacier effect) suggests active/
fresh bleed.
|

|
|
Hypodense
bubbles within the hematoma suggest venous tear.
|
Biconvex EDH-CT
|
|
The hematoma may become isodense in about 2 weeks.
Obliteration of cerebral sulci may give a clue.
A chronic EDH may reveal a contrast enhancing periphery.
Associated parenchymal injury, and a midline shift of
>8mm suggest a bad prognosis.
|
|
|
MRI scans show better delineation of the pathology. The displaced
dura
|
Fracture
& contra-coup EDH-CT
|
|
appear as a thin
low signal intensity between the hematoma and brain.
Ultrasound is
useful in children with open fontanels and cost effective during
conservative treatment and follow-ups.
Management:
Non operative management may
be tried when an EDH is an incidental finding and small (<1cm) with
no suggestion of raised ICP or focal deficit.
|

|
|
Close
observation with serial CT scanning is a must.
|
Post.fossa EDH-CT
|
Prolonged hospitalization may be required.
In an emergency when clinical symptoms develop rapidly and
an urgent CT scanning is not available, exploratory burrholes
on the site of fracture or soft tissue injury and/or in the temporal
region on the side of pupillary dilatation are carried out.
Frontal and parietal burrholes may be done if the other burrholes
do not reveal a clot. It is advised to explore the opposite side as
well. However, burrholes usually do not lead to radical removal of
the EDH.
A craniotomy allows radical removal of the EDH
and control of the bleeding; the dura may be opened if associated SDH is
suspected. Bony decompression is advised by some surgeons. Some surgeons
prefer to leave a drain. A ventricular drainage may be required in
posterior fossa lesions.
Massive (malignant) cerebral edema following
evacuation is assumed to be due to loss of cerebral autoregulation. It is
usually associated with delayed evacuation and very difficult to treat.
Post operative intensive management with attention to
metabolic, respiratory, and infective complications associated with
prolonged unconsciousness determines the final outcome. ICP monitoring
helps to detect reaccumulation of the EDH.
Prognosis:
It depends on the extent of secondary brain injury and
associated injuries. The nature of the first aid given and the timing of
the surgery determine the prognosis. The longer the period of lucid
interval, the greater are the chances of full recovery. GCS at the
time of surgery, and the volume of EDH also determine the
outcome.
The overall mortality ranges from 20-40% in various series.
Children do better. Faster transportation of the head injured, earlier
recognition of the clot, improved neurosurgical services, and the
availability of CT scans have greatly improved the prognosis.
|