|
Brainstem was, not long ago, considered
as a 'no man's land'.
With recent advances in neuroimaging,
and surgical tools, there is a renewed interest in brainstem tumors among
neurosurgeons.
All brainstem tumors do not behave in
the same manner. In the past, all tumors of the midbrain, pons, and
medulla oblongata were regarded as 'brainstem tumors'. Recently, it has
been suggested that there is a distinction between the thalamic and
midbrain lesions on the one hand and pons and medulla lesions on the
other and that the brainstem gliomas are not a homogeneous group with
regard to their clinical, pathohistological, or biological features and
that their prognosis may be directly related to tumor type and location.
Pathology:
Brainstem tumors are most commonly
diagnosed in children, in whom they account for 10% to 20% of the primary
brain tumors.
Pilocytic astrocytomas account for 30%
of all infratentorial tumors in childhood, and 80% of pilocytic
astrocytomas are found in the posterior fossa. The reported increase in
the incidence of primary malignant brain tumors in children by 35% from
1973 to 1994, appears to be brainstem tumor rates, which may due to
advances in imaging.
Brainstem gliomas have been classified
by site, imaging, and pathology.
However, in clinical practice, they are
classified into diffuse, and focal ones; both may have exophytic growth.
The diffuse type accounts
for nearly 80% of them. The majority arising from and causing diffuse enlargement
of the pons. Axial and exophytic growth is also found in two thirds of
the cases. The medulla is often spared.They are infiltrative in
nature with relentlessly progressive. They present with short duration of
symptoms, usually consists of multiple bilateral cranial nerve deficits.,
long tract signs, and ataxia. Raised ICP and hydrocephalus are rare and
occurs in 10% of cases.
Histologically, they belong to
fibrillary astrocytomas, anaplastic astrocytomas, and glioblastoma
multiforme.
Focal ones may be
discrete (<2cm in diameter) and exophytic variants.
They may be cystic or solid.
Cervicomedullary variants arise
from upper cervical cord, with typical rostal extension into the
cervicomedullary junction. The rostal extension is limited anteriorly by
the pyramidal decussations; thus the mass expands posteriorly at the
level of the obex and may rupture into the fourth ventricle. The caudal
part is identical to an intramedullary tumor. They usually present with
lower cranial nerve deficits, long tract signs, and occasionally
torticollis.
The dorsal exophytic variants
arise from the floor of the fourth ventricle, usually filling it.
Clinically, there is marked by an insidious failure to thrive and signs
and symptoms of raised ICP in the young. Cranial nerve deficits are found
in 50% of them; but long tract signs are rare.
Histologically, they mostly belong to
pilocytic astrocytomas.
|
Imaging:
Radiological findings
associated with low grade tumor include, the presence of exophytic
protrusion into the fourth ventricle through the dorsal brainstem and
cervicomedullary location, and surgery has been recommended.
On MRI, the focal tumors are
small, well circumscribed without associated edema or evidence of
infiltration. Cystic changes may occur. The diffuse ones are hypodense
on TI and hyperdense on T2.
Differential diagnosis include,
|
|
|
|
|
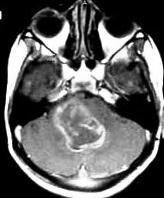
Exophytic type with necrosis
|
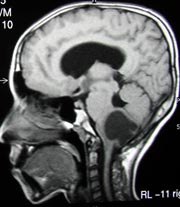
Cervicomedullary
cystic type
|
|
focal: ependymomas, tuberculosis, metastasis, lymphoma,
abscess, vascular malformations, and infarction.
diffuse: vascular malformations, demyelinating lesions, and encephalitis.
Some of them may disseminate. Neuroaxis
imaging and CSF analysis, if possible, have been recommended.
Management:
Surgery, despite all
the recent advances, has
limited role in diffuse ones.
Resection of well circumscribed, low
grade tumors has been shown to improve survival.
Cystic components, and focal tumor
appearance are thought to be favorable features for surgery.
Exophytic ones may be amenable for
surgery; patient selection is critical.
A midline suboccipital approach is
commonly preferred. Lateral exophytic ones may need a CP angle approach.
The floor of the fourth ventricle, or
the lateral brainstem in CP angle approach, is inspected for bulges and
discoloration.
Cyst, if any, should be aspirated .
Exophytic area, if any, is incised.
Methylprednisolone may be given just before incision, and continued for
24 hours (30mg/kg for the first hour followed by 5.4mg/kg/hr.
If no exophytic area is seen, one of the
'safe areas' is incised longitudinally, after mapping out eloquent areas
by direct electrophysiological stimulation of the cranial nerve nuclei.
Continuous intraoperative EMG monitoring from certain muscles of the head
is an alternative and can provide information about the status of the
respective cranial motor nerves.
The tumor is excised in piecemeal with
meticulous microsurgical techniques; recent tools, such as laser,
irrigation bipolar,and ultrasonic aspirator, facilitates tumor excision.
Tumor rim may be left behind, if there is no satisfactory cleavage is
seen.
In view of the wide variety of brainstem
lesions, a tissue diagnosis is warranted for appropriate treatment.
The use of open biopsy, and more
recently, image guided stereotactic biopsy has been advocated for tissue
diagnosis. In addition, cyst, if any, may be drained which will help
symptomatically.
Stereotactic biopsy is indicated in focal
enhancing masses, especially when open surgery was not contemplated, for
whatever reason.
Stereotactic procedures make use of
a transfrontal trajectory, through the axis of brainstem, for biopsies of
the diencephalon, midbrain, and rostal pons, and
a suboccipital transcerebellar trajectory, through the middle cerebellar
peduncle, for biopsies of the lateral pons.
Steretactic biopsy is generally not
advised in dorsally exophytic tumors, cervicomedullary tumor, and focal midbrain
tumors.
Open surgery has been suggested as a
better option.
A stereotactic biopsy is unreliable in
diffuse non enhancing tumor. Diffuse ones has image characteristics which
are almost diagnostic, and the stereotactic biopsy, especially in
children, is not reliable in the diffuse variety. Direct radiotherapy is
acceptable without biopsy.
Aggressive radiotherapy and chemotherapy are recommended as alternatives, in
diffuse ones; the standard therapy has been 55Gy to the tumor area with
weekly dose of 800-1000 cGy.
Prognosis:
Prognosis is generally poor in children.
Adults do better.
Small size, lack of diffuse appearance,
accessible location, and absence of preoperative neurological deficit
suggest favorable outcome. Some have questioned the value of surgery;
they claim the better prognosis is due to histology which is mostly
pilocytic in focal and exophytic variants.
Most authors agree that there is little
improvement in survival, with the attempted resection of a high grade
tumor, even though in specific instances current advanced techniques
allow for the performance of such surgery with acceptable morbidity.
Two year survival is reported to be 18%
to 46% with radiotherapy in diffuse ones.
Chemotherapy, when added to radiotherapy
results a median survival of 44 weeks and a 1 year survival of 47%.
Other modes of radiotherapy do not add
to it. Experience with radiosurgery is limited. SRT is, usually,
preferred.
|