|
It is a
abnormal communication between carotid arteries and cavernous sinus.
Classification:
They may be
traumatic or spontaneous, high or low flow, direct or dural fistulae as
determined by angiography.
Angiographic
classification is widely followed and helps in the treatment planning.
- Type A- is a direct shunt from the internal carotid to the
cavernous sinus.
- Type B- is between the branches of internal carotid and the
sinus.
- Type C- is between the branches of the external carotid and
the sinus.
- Type D- is between the branches of both internal and
external carotids and the sinus; it is the commonest.
Etiology:
Traumatic
fistulas are the commonest (75%) with
a male preponderance. They are high flow fistula.
Severe
closed head injury is the commonest cause. Penetrating injuries rarely
cause the fistulas.
Post
surgical (transphenoidal procedures, percutaneous Gasserian rhizotomy,
intracranial carotid embolectomy) causes are
very
rare.
Spontaneous fistulas are low flow ones and account for 20%, occurring
in the older age group with a female preponderance.
Exact
cause is not known. It may be congenital as in other AVMs or may be due
to micro traumatic rupture of the meningeal
branches
of the carotids.
Intracavernous
carotid artery aneurismal rupture constitute a minor group (5%)
and are more common in females, presenting
as
spontaneous fistula. They may be high or low flow depending on size of
rupture.
Pathology:
The
cavernous sinus is distended along with the superior orbital vein and
the sphenoparietal sinus leading onto intraorbital
swelling
and hence proptosis which is down and out. Stasis contributes to
chemosis, conjunctival edema and prolapse.
Reduced
perfusion pressure in the ophthalmic artery and the increased
intra-orbital and venous pressure leads to retinal
ischemia
and blindness; there may be vitreous hemorrhage, papilledema and in
chronic stage, glaucoma.
Severe
proptosis may lead to corneal ulcerations and perforation of the globe.
|
Clinical
features:
The symptoms
and signs depend on the type, size and site (either anterior or
posterior) of the fistula.
Type
A are usually high flow and due to
trauma or rupture of intracavernous carotid aneurysm. They do
not close
spontaneously
and require active treatment. Pulsating exophthalmus, chemosis, ocular
nerve palsies causing diplopia, visual
loss and
exposure keratitis are the usual manifestations. Facial pain due to
involvement of cranial nerves V1 and V2 may be
there. Flow
through cortical veins may produce raised ICT and headache.
A
subjective and audible bruit may be present.
The ocular
signs may be bilateral or contralateral due to the intercavernous
communications.
A CCF is
seldom fatal. Associated tear of the lateral intracranial dura can lead
to subdural or subarchnoid haemorrhage.
In spite of
extensive steal from the intracranial circulation, hemispheric signs are
rare.
In type
B, C, D, the symptoms are mild and of insidious onset; may be self
remitting.
|
Investigations:
CT
and MRI may suggest a
distended cavernous sinus and rule out other causes of ocular
manifestations. They may also help to study the extent of skull
fracture, if any.
Angiography is the preferred imaging. Selective internal and
external carotid studies will help.
Transcranial
Doppler and SPECT scanning help in assessing tolerance
in carotid occlusion.
|
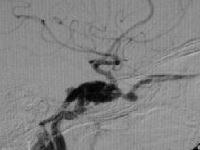
Type A CCF- angio
(Lat)
|
Management:
The
indication for active intervention is the progressive visual loss. Types B,
C, D are low flow and reported to close spontaneously in 16 to 60%.
Angiography alone may promote spontaneous closure, it has been reported.
Protection of the eye during the waiting period is advised.
Active
intervention is indicated in progressive symptoms. The aim is to occlude
the fistula without occluding the internal carotid either by embolization
or surgery.
Type A can
be closed by embolization either intraarterial through the internal carotid or
intravenous through the superior ophthalmic vein or the superior or
inferior petrosal sinus through surgical exposure; direct surgery may be
required in the failed cases.
Type B is
rare and requires direct surgery usually.
Type C is
also rare and can be embolized.
Type D is
the commonest; External carotid feeders may be embolized and internal
carotid feeders may require surgery.
Surgery
may involve ligation of the carotid (CCA
or ICA) in the neck, trapping of the cavernous segment of the carotid, both
proximally and distally or direct exposure of the lesion and micro
reconstruction of the involved segment which is a surgical challenge.
|