|
The C-V junction is a
transition site between mobile cranium and relatively rigid spinal
column. It is also the site of the medullo spinal junction. CV anomalies
are defects of development, not necessarily congenital and may not
manifest at birth.
Development:
It is a complex process.
Mesodermal somites numbering
42 appear at the 4th week
Ventromedial part of the
somatomes migrate and cluster around notochord-Sclerotomes
A fissure in each sclerotome
separate a denser caudal half from loosely arranged cranial half.
Caudal half joins with
cephalic half of adjacent sclerotome - future vertebra
Mesenchymal cells of the
fissure condense to form I.V.D.
Notochord disappears at the
vertebral bodies, but persist as disc (nucleus pulposus)
This membranous stage is
followed by chondrification and ossification.
Out of 4 occipital
sclerotomes the first 2 form basiocciput, the III Jugular
tubercles and the IV (Proatlas) form parts of foramen magnum,
atlas and axis.
Dysplasia of the occiptal
segments may flatten the clivus - platybasia.
When the basiocciput and rim
of foramen magnum are underdeveloped, the odontoid and arch of atlas may
grow normally to over hang along the sides. Odontoid and arch of atlas
invaginate-Basilar invagination.
The proatlas may develop
into separate vertebrae - Occipital vertebra, hypochondral bow of
proatlas may persist to gain attachment to the atlas, clivus or even to
the apical segment of the dens - responsible for anti-cervico medially
compression.
The axis has a fully
developed center from the second sclerotome which form the caudal part of
the body and articular facets.
At birth odontoid base is
separate from the body of axis by a segment of cartilage which persists
until the age of eight and the center gets ossified., may remain separate
as Os- odontoidium.
The apical segment is not
ossified until 3 years of age. At 12 years if fuses with odontoid to form
normal odontoid., failure leads to Os terminale.
Classification
CV anomalies:
|
Developmental
|
Genetic
and miscellaneous:
|
|
Malformations of
occipital bone:
Clivus segmentation
Remnants around
foramen magnum
Basilar
invagination
Condylar hypoplasia
Abnormal occipto
atlantal ligament
Malformation of
atlas
Failure of
segmentation from occiput
Atlanto axial
fusion
Aplasia of atlas
arches
|
Malformation of
axis
Irregular
atlantoaxial segmentation
Dens dysplasias
Ossiculum terminale
persistence
Osodontoideum
Segmentation
falilure of C2-3
Neural dysgenesis
|
Errors of
metabolism
Down's
syndrome (lax joints)
Achondroplasia
|
|
|
|
Often the anomalies are in
different combinations and hence the difficulty in an appropriate
terminology in every case. Certain terms are conventionally used to
express the anomalies, as follows
1. Platy basia:
Flatness of the base of
skull. Angle formed by the clival line and a line drawn along the floor
of ant. cranial fosse exceeds 140 degrees.
Platy basia alone not
associated with other conditions does not produce any symptoms.
2. Basilar
Invagination:
Vertebral column invaginates
into the posterior fossa which is of 2 types:
The anterior type has a
short clivus horizontally placed, with the anterior lip of the foramen
magnum invaginated in relation to the spinal column.
The other is paramedian
invagination associated with hypoplasia of the occipital condyles. Thus
the atlas may get invaginated. The hypochondral bow of the proatlas may
persist to gain articulation or fusion with lower end of clivus, ant.
arch. The mass of bone may cause ant. compression. There is associated
soft tissue anomalies of hind brain in 25-30% of cases. In certain
diseases of bone like hyperparathyroidism, pagets or osteomalacia, there
is softening of the base of skull which gets invaginated. This is called
basilar impression or secondary basilar invagination.
3. Assimilation of
atlas:
Assimilation of atlas with
the occiput is an expression of nonsegmentation of certain parts of the
proatlas and fusion of the first spinal sclerotome with the proatlas. It
occurs in 0.25% or less. However its occurrence along with other CV
anomalies is frequent. It could be partial or complex and may restrict
occiptial movement. It is frequent in Klippel-feil syndrome, involving
the second and the third vertebral bodies and may affect the atlanto axial
joint. This combination of assimilation of atlas and segmental failure of
the II and III vertebral bodies exert an abnormal strain on the atlanto
axial joints from childhood. In course of time the ligaments become lax
and mobility increases predisposing to atlanto axial dislocation.
4. Os Terminale:
Refers to the nonfused
terminal part of the odontoid derived from the centrum of the IV
occipital sclerotome. This apical segment is usually about 12mm in
length, but can be very small. In case of disruption at the interface and
if atlanto axial dislocation occurs, the remaining part of the odontoid
may compress the cervico meduallary region.
5. Os odontoideum:
This term has been used to
denote a separate piece of bone present posterior to the anterior arch of
atlas. The odontoid base fails to fuse with the axis. These are only few
odontoid base falls to the above specification. But the diagnosis of Os
odontoideum is much more frequent in clinical practice. Careful exam
reveals a small hypoplastic odontoid at the upper border of the body of
the axis. It is generally believed that traumatic fracture leaves an
irregular margin, though the margin may be rounded enough to be
indistinguishable from the developmental anomalies. Many of the patients
have history of fall. Dens lacks a good nutrient artery. Blood supply
thro' the body of axis is limited due to interposition of cartilage
between body and the odontoid process. An injury in early childhood probably
leads to Os-odontoideum in later life due to avascular necrosis. In the
absence of strong reasons to consider embryological basis, traumatic
theory is more rationale.
Pathogenesis of
Neural involvement:
Neural involvement is
basically due to 3 mechanisms.
Mal aligned bony components
of the spinal canal compress underlying cord due to dislocation of the
joints, the commonest is Atlanto axial dislocation.
Encroachment into the spinal
canal may also occur due to formation of the abnormal bone masses around
the CV junction. Occasionally the foramen magnum may be narrowed or the
rest of arch of the atlas may be deformed to cause compression of spino
medullary junction.
Lastly, associated Chiari
malformation and syrinx may cause further neural compression.
A-A dislocation is the
commonest abnormality, be it congenital or acquired. A dysplastic
odontoid provides a vulnerable situation. The transverse ligament may be
basically in- competent or become so after a minor trauma. If the
dislocation is sudden and severe, an acute quadriparesis may occur.
Abnormal mobility in flexion may cause transient neural compression
resulting in sudden transient deficit and occasionally Lhtermitte's
sign. In course of time the dislocation may become fixed leading to
progressive deficit. If it goes on for years vascular damage may happen
with no recovery even after adequate decompression. Deformities involving
the facet joints between atlas and axis may give rise to rotatory
dislocation . Such deformities cause only a neck tilt and pain without
neuro deficit.
Occipito-atlantal
dislocation is rare.
In basilar invagination,
there is crowding of structures in the small post. fossa resulting in
compression of medulla, long tract involvement and lower cranial nerve
deficits. Rarely there is vertebral art. compression leading onto VBI.
Clinical features:
Prevalence appears to be
high as observed by neurosurgeons in India although it is yet to be
corroborated by epidemiological studies. The abnormalities may have a
familial occurrence. In one series they affect children and young adults
primarily. Majority of patients present in their second or third decade.
There is male preponderance (1:5:1). H/o. trauma is often available. Many
children have URI preceding the onset of symptoms.
Symptoms:
Progressive weakness of
limbs, stiffness, difficulty in walking and neck pain are the modes of
presentation in 75-85% of cases. Smaller number present with neck tilt,
neck pain, cough headaches, occipital cephalalgia without any deficit. Symptoms
of lower brain stem dysfunction, such as dysphagia, dysphonia, nasal
regurgitation, sleep apnoea are due to basilar invagination.
Signs:
Physical appearance is often
striking. Short stature, short neck, low hairline, head tilt, facial
asymmetry, web neck, or scoliosis occur in different combinations.
High arched palate,
hemiatrophy of tongue, and syndactyly may be associated. Evidence of high
cervical cord compression with or without sensory involvement is common.
Involvement of one limb or one sided limbs may be misleading . Crossed
hemiparesis may suggest cervico medullary junction involvement. Small
muscle atrophy due to 'central cord syndrome' like effect of the lower
cord level due to upper cord compression is seen in 22%. Spino thalamic involvement
is uncommon. Posterior column involvement is seen in 60%. Sphincter
disturbance is rare. Associated syrinx may produce dissociated or
suspended sensory loss. Lower cranial nerves are involved in about 18%.
Cerebellar involvement is seen in about 16%. Mirror movements of the
hands are often seen in klippel Feil syndrome due to inadequate
decussation of pyramidal tract at medulla.
Imaging:
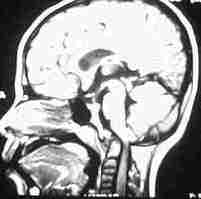
MRI has totally changed the
prospects of investigation of spinal lesions and more so at CV junction.
The soft tissue details can be imaged with a high degree. CT scan with
reconstruction is still preferred by some to study bone details. X ray
with chamberlin line, mcgregor line etc have become history.
|

|

|

|
|
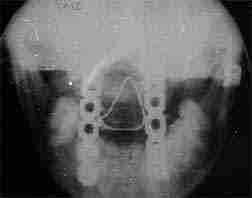
Atlanto-Axial
subluxation
|
platibasia
|
basilar
invagination(odontoid at the level of IAM)
|
|

|
|

|
|
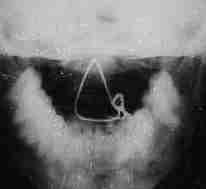
3D CT transoral
view of odontoid(basilar invagination)
|
AP view
|
lat. view
|
|
posterior fixation with wiring and plating after odontoidectomy
|
Management:
Though a number of bony and
ligamentation anomalies have been described, consequences are mainly due
to (A) A -A dislocation (B) malformed components of bone producing
compression.
In early stages of A-A
dislocations, most of them are reducible and require only stabilization.
Irreducible types require
open reduction (operative reduction). Operative treatment has involved
thro' several modifications. The first effort was in 1910 by Osgood, who
tried to reduce the dislocation by pushing backwards the atlas via the
pharynx while the posterior arch of atlas was pulled back with a thick
silk thread, which was then tied to spinous process of axis. This was the
beginning.
Gallow popularized the
technique of midline wiring which kept the atlas and axis is opposition.
The wire retains an interposed only bone draft. Several modification were
suggested. Screw fixation of facet junctions, Halifax clamps, contoured
rods are the latest. Hartshell frame is still being used by many. Some have
recommended methylmethacrylate use. All these methods are effective when
reduction of dislocation is adequate.
Instances of redislocation
by snapping of wire, loosening of screws are not rare.
In the fixed or irreducible
variety foremen magnum decompression along with C1 & C2 laminectomy
is recommended by few and claim to have satisfactory results, if done
after a period of skull traction. Oppel was probably the first to operate
by ant. route.
Removing the compressing element form it front is more rationale.
Recently this has become the
preferred procedure. The arch of the atlas, the odontoid and part of the
axis can be excised. In addition, the thick ligament and chronic
granulation tissue which contribute to compression can be excised.
The ant aspect of CV
junction can be approached by Trans pharyngeal, Transpalato pharyngeal, Trans
maxillary (Le fort - with maxillary down fracture) routes.
It is generally accepted that a stabilization procedure is necessary
following ant. decompression either in the same sitting or as a II stage
procedure. Of late ant. stabilization following decompression has been
tried in some centers. Some feel a stabilization procedure is not
required in selected cases.
|
|
|

|
|
Basilar
invagination - Achondroplasia
|
AP view
|
LAT
view
|
|
posterior wiring
after odontoidectomy
|
Irrespective of methods used
it is essential to immobilize its CV junction with collar till bony
fusion occurs, which may take 3 months. Ideal will be the Halo frame.
Outcome:
Significant relief in 70% of
cases following ant. decompression can be expected. Reduction in
spasticity is appreciated in the immediate post operative period.
Fatal meningitis, post
operative dislocation are possible complications.
|