|
It is group of
tumors with similar histological appearance that are thought to arise
from germinal or matrix cells of the primitive embryonal neural tube.
Ependymoblastomas, rare, malignant, tumors with distinct ependymal differentiation,
are included together with medulloepitheliomas, neuroblastomas,
ganglioneuroblastoma, pineoblastoma, and medulloblastomas in the group of
embryonal tumors.
In the past, these tumors, along with
medulloblastoma, were included in 'Primitive Neuroectodermal tumors
(PNET)'.
Recently, WHO reserved the term PNET only to Medulloblastoma,
irrespective of location.
The majority of
these embryonal tumors are found infratentorially in the form of
cerebellar medulloblastomas.
Other embryonal
tumors are predominantly large tumors, often involving the deep
supratentorial structures. The children are most commonly affected. In
children, they account for 2.5% to 5% of all primary brain tumors.
|
They have
a well known propensity to disseminate, occasionally doing so
systemically.
They
resemble each other histologically.
Histologically,
they are composed of a sheet like pattern of undifferentiated cells
containing dark, oval to irregular nuclei surrounded by minimal amounts
of cytoplasm.
Variable
degrees of neuronal and glial differentiation may be observed.
Naming of
the individual tumors within this category depends on histology.
In cases
of neuronal differentiation (Homer Wright rosettes), it is 'cerebral
neuroblastoma'.
In cases
of ganglion like morphology, it is 'ganglionneuroblastoma'.
In cases
with differentiation along multiple cell lines, it is 'mixed
malignant tumor'.
|
|

|
|
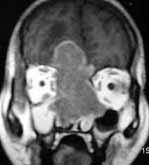
Ependymoblastoma-MRI
|
|
In cases with
ependymal differentiation (perivascular pseudorosettes and true
rosettes), it is named 'ependymoblastoma'..
Seizures and focal
neurological deficits, with features of raised ICT are the symptoms at
presentation.
CT and MRI reveal
a well differentiated, heterogenous, markedly enhancing hemispheric mass
with varying degree of cystic or necrotic changes. Evidence of CSF
dissemination is typically seen as focal or diffuse enhancement within
the subarchnoid space and ventricular system.
Aggressive
multimodality approach, similar to the management of medulloblastomas, is
recommended.
Complete
resection, and post operative craniospinal radiation is commonly used.
Chemotheray have
taken a greater role in children.
The prognosis is
poor, with few survivors beyond three years.
Medulloepithelioma:
This
is an extremely rare tumor, possibly derived from the primitive medullary
plate and neural tube. Rubinstein considers it the most primitive
and multi-potential neoplasm in neuro-oncology and a truly ‘embryonic
tumor’.
The
tumor is essentially cerebral in location and is generally encountered
early in life.
It
is usually soft, friable and hemorrhagic.
Microscopically
it presents a papillary and almost tubular arrangement of medium or tall
columnar cells, recalling the structure of the primitive medullary
epithelium. These cells are bounded by an internal limiting membrane
and may be arranged in a single layer and show slight
stratification. Neither cilia nor blepharoplasts can be demonstrated
and the nuclei are large, oval and vesicular. The papillae and
occasional solid cords of tumor cells rest on a prominent vascular
connective tissue stroma which might be so proliferated as to create the
impression of an additional vasoformative tumor.
Generally,
these primitive tumors do not exhibit any cellular maturation, but
occasionally there may be evidence of a neuroblastic transformation in
the majority of tumors. However, tissue culture experiments
have shown that medulloblastomas are uniformly neuroblastic in virto.
Neuroblastoma:
Neuroblastomas
are rare tumors occurring essentially during the first year of
life. Many occur as congenital tumors. These arise from immature
neurons and characteristically, therefore, possess the ability to mature
into adult neurons. Another feature is their ability to
undergo arrest of maturation and involution.
They may arise
in two situations, viz., cerebral and olfactory. Though extracranial
examples are more common than cerebral forms, the histological features
are similar in both regions.
|
Cererbral neuroblastomas are found
most frequently in children, under 5, and situated deep in the brain
often in the forntoparietal lobes, where they form a defined mass.
Histologically, it consists of a pattern less proliferation of small
cells often engaged in Homer-Wright resettes similar to those observed
in medulloblastoma, but glial differentiation is not seen.
Olfactory neuroblastoma (Esthesio
neuroblastomas) are peculiar tumors that arise from the olfactory bulb
or more frequently from the roof of the nasal cavity. They spread
locally along the paranasal sinuses and may invade the frontal lobe.
The treatment consist of surgery and radiation. They are highly
radiosenstive.They tend to recur. Long term survival is possible.
|
|
|
|
Esthesio neuroblastoma
|
|
The
histological features are comparable to those of cerebellar
medulloblastoma. Generally, a highly cellular neoplasm is seen and
this consists of fairly uniform cells resembling the cerebellar
medulloblastoma, with scanty cytoplasm and a large deep-staining
nucleus. Homer-Wright rosettes may also be seen in up to 50 per
cent of cases. In many areas, islands of cells may be separated by
strands of connective tissue. Silver stains may show the presence
of neurofibrillary material and in some areas, cells suggestive of
immature neurons may be seen. Secondary changes such as necrosis,
hemorrhage and calcification are rare. The undifferentiated variety
has sheets of small tumor cells with dense circular nuclei. With
greater differentiation vaguely defined rosettes or small clusters of
cells may be seen in places. In either event, the tumor shows a
considerable amount of connective tissue, specially a rich reticulin
framework, which reaches up to the surface arachnoid mater. On this
account, the cerebral neuroblastoma, like the medulloblastoma, may be
confused with a meningeal sarcoma. Parts of the tumor may show some
differentiation towards the formation of neurons.
The tumors are of low grade malignancy
and the olfactory examples are of relatively slow growth. Though
highly radiosensitive, they are liable to recur and spread to adjacent
regions. The olfactory neuroblastoma (esthesioneuroblastoma) may
possibly have its origin in the olfactory bulb and present as a
paramedian frontal space occupying lesion.
Recurrence after surgical removal and
changes in histological features after radiation have been described.
Medulloblastomas:
discussed elsewhere.
Pineoblastomas: discussed
elsewhere.
|