|
Dural AVMs are abnormal arteriovenous connections lying
within the dura; they are rare, representing about 10% of all
intracranial AVMs.
Pathology:
They are thought to be acquired rather than congenital.
There is an association with previous trauma, infection, craniotomy and
sinus thrombosis.
Two theories of development are in vogue:
a) Venous sinus thrombosis followed by attempted
recanalisation leading to opening of embryonic arteriovenous
communications.
b) Single AV channel causing turbulent flow leading to sinus
thrombosis followed by recruitment of arterial and venous connections.
Various sites may be involved, most commonly the lateral and
cavernous sinuses (type B, C, and D CCFs).
Other sites include the floor of the anterior cranial fossa, superior
sagittal sinus, inferior petrosal sinus, the tentorial incisura,
torcular, and the craniocervical junction. Occasionally they may be
multiple. The arterial feeders are meningeal branches of the internal or
external carotid and vertebro-basilar arteries and venous drainage is to
the nearest sinus and occasionally to the pial veins.
Under pathological conditions, these channels are
transformed into retrograde venous drainage pathways from the
arterialized dural leaflet into the adjacent leptomeningeal circulation.
The resulting retrograde leptomeningeal venous drainage becomes
progressively tortuous and eventually becomes varicose or aneurysmal. It
is this retrograde leptomeningeal drainage that is associated with most
of the neurological sequelae.
Some lesions undergo spontaneous involution and resolution.
Clinical features:
Many of these lesions remain asymptomatic.
Symptoms depend on the site; they are due to arterial and
venous phenomena.
25% show aggressive tendency with hemorrhage or focal
deficits, especially those at tentorial incisura, anterior cranial fossa
floor and the sagittal sinus. Those with pial venous drainage and
aneurismal dilatation of the draining veins are more likely to be
aggressive.
CCFs present to the ophthalmologists with ocular signs and
symptoms.
Lateral sinus fistulae may present with tinnitus,
fluctuating visual disturbances, raised ICT.
Superior sagittal sinus fistulae present with headache,
hemorrhage, stroke, dementia and cortical blindness.
Anterior cranial fossa lesions present with hemorrhage and
visual loss.
Cranial bruit may be heard in 40% with tinnitus.
Patients may also present with SAH or ICH.
Investigations:
CT and
MRI may show dilated cortical veins
without parenchymal
nidus; associated hemorrhage and infarction may be seen. MRA may
be useful on occasions.
Selective angiography of both internal and external
carotids is the imaging of choice. Normally the dural arterial
branches are not seen in angiogrphy; but the DAVMs are well visualized.
|
|

|
|
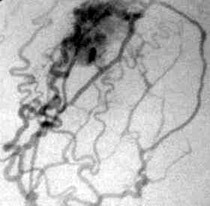
DAVM-dural supply
(Ext.Carotid angio)
|
DAVM- Pial & dural supply
in common carotid angio
|
Management:
Symptomatic ones obviously need to be treated.
Incidental, asymptomatic ones must have angiographic
evaluation to assess the risk of hemorrhage; if the risk is significant,
they should be treated.
Obliteration of the nidus should be the aim.
Simple interruption of the feeders will lead to recurrence.
Surgical excision of the nidus, and the involved sinus in
addition to the ligation of feeders carries 15% mortality,
depending on the site involved.
Endovascular techniques are increasingly
used these days. The persistence and recurrence rates after transarterial
embolization alone are high. Therefore,it is reserved for palliative
measure and as a preoperative adjunct to diminish the flow through the
the fistula. Lately, transvenous endovascular therapy has markedly
improved the cure rate and become the treatment of choice.
More recently, radiosurgery has been shown to be successful in
treating these fistulae. Long term studies are awaited.
|